TIP(S)ing the scales against portal hypertension
What is a TIPS?
A transjugular intrahepatic portosystemic shunt, or TIPS, is a low-resistance shunt created between one of the hepatic veins and an intrahepatic branch of the portal vein. A TIPS decompresses the portal venous system by bypassing the liver and allowing blood to return to the systemic circulation.
During a TIPS procedure vascular access is obtained through the right internal jugular vein. A catheter is advanced into the right or middle hepatic veins and, using intravascular ultrasound or carbon dioxide portovenogram, an intrahepatic segment of the portal vein is targeted. The TIPS needle and catheter are advanced through hepatic parenchyma into the portal venous system and the intrahepatic tract is balloon dilated. The TIPS shunt is then created by deploying a mental stent.
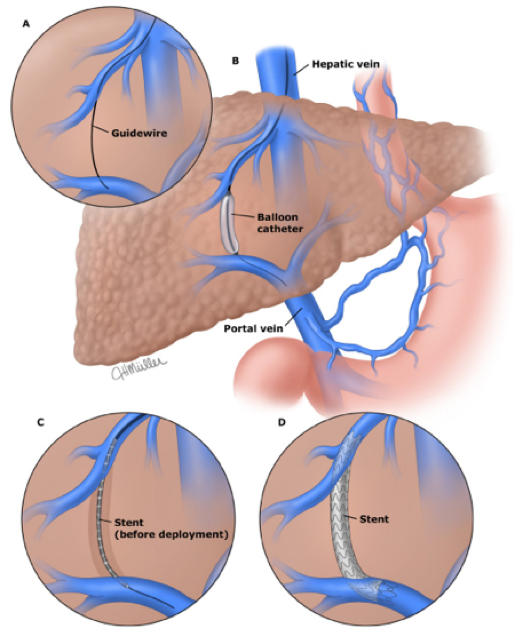
Figure 1: TIPS procedure. Image taken from: Bajaj JS, Sanyal AJ, Collares FB. Overview of transjugular intrahepatic portosystemic shunts (TIPS). In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA.
During the TIPS procedure, portal venous and free hepatic vein pressures are obtained pre- and post-TIPS to calculate the pre- and post-TIPS hepatic venous pressure gradient (HVPG). Ideally, the TIPS stent is dilated until a post-TIPS HVPG of <12 mmHg is achieved. An HVPG of <12 mmHg has been shown to significantly decrease the risk of variceal bleeding.Embolization of gastric varices may be required to prevent early rebleeding despite adequate decompression of the portal venous system.
Pre-TIPS evaluation
Prior to TIPS placement lab tests should be drawn to calculate the pre-TIPS MELD score. Patients with a MELD score of >18 or serum bilirubin >4.0 mg/dL have a higher risk mortality at 3 months after TIPS and TIPS should only be performed in the absence of other options and after patients are informed of their prognosis.
Cross sectional liver imaging with CT scan or MRI should also be performed prior to TIPS placement. Imaging should assess portal and hepatic vein patency, spleen size, ascites, and evaluate the extent of portosystemic collaterals.
In patients with signs, symptoms or a history of congestive heart failure, tricuspid regurgitation, cardiomyopathy or pulmonary hypertension a cardiac evaluation should be performed prior to TIPS. Most commonly, this includes a cardiac echo with cardiology or pulmonology consultation as necessary.
What are the indications for TIPS?
Variceal bleeding
Patients with actively bleeding esophageal varices refractory to pharmacologic and endoscopic therapy are candidates for portal decompression with TIPS. The urgency of TIPS placement is an independent predictor of mortality, however. TIPS has been shown to control bleeding in 90-100% of actively bleeding patients with rebleeding in only 6-18% but a 6-week mortality of 15-50%.
After a variceal bleed the risk of rebleeding is >50% with each bleeding event carrying a significant mortality rate. TIPS has been shown to decrease the rate of variceal rebleeding compared to endoscopic therapy but carries a higher risk of hepatic encephalopathy with no improvement in overall survival. As a result, TIPS is only recommended in those who fail pharmacologic and endoscopic therapy after their first variceal bleed.
Table 1: TIPS versus endoscopic + ß-blocker therapy after 2 years follow-up.Table adapted from: Holster IL, Tjwa ETTL, Moelker A, et al. Covered transjugular intrahepatic portosystemic shunt versus endoscopic therapy + ß-blocker for prevention of variceal bleeding. Hepatology 2016; 63(2): 581-589.
Emerging data does suggest that patients who are at high risk for rebleeding after their initial EV bleed (Child-Pugh class C, Child-Pugh class B with active bleeding on endoscopy despite vasoactive therapy, or HVPG >20 mmHg) may benefit from early TIPS placement within 72 hours of endoscopic therapy, though subjects were highly selected for inclusion in the cited study.In one meta-analysis of eleven randomized trials, TIPS patients had a higher rate of transplant-free survival at two years (79% vs 64%) with no difference in rates of hepatic encephalopathy.Additional studies are needed to corroborate these results.
Compared to esophageal varices, gastric and ectopic varices (duodenal, stomal and anorectal) can be more technically difficult to treat. Cyanoacrylate injection is the preferred initial treatment for gastric varices but TIPS is an alternative for those who have failed or are at high risk of failing endoscopic therapy. In small studies BRTO has been shown to be more effective than cyanoacrylate to prevent re-bleeding from ectopic varices and BRTO can be considered as an alternative to endoscopic treatment or TIPS but additional research is needed. TIPS is the preferred approach to prevent rebleeding in ectopic varices.
Ascites
Ascites are defined as refractory to medical treatment when they are unresponsive to sodium restriction and high-dose diuretics (spironolactone 400 mg/day and furosemide 160 gm/day) or patients are intolerant to diuretics. Refractory ascites carry a poor prognosis with 50% mortality rate at 12 months. Compared to repeated large-volume paracentesis, TIPS carries a higher risk of encephalopathy with uncertainty as to any difference in survival. As a result, TIPS can be considered for refractory ascites after a careful discussion of risks and benefits compared to serial large-volume paracentesis.
Budd-Chiari Syndrome
Hepatic venous outflow tract obstruction at the level of the hepatic vein or inferior vena cava can result in acute liver injury or failure from hepatic congestion. Initial treatment for Budd-Chiari syndrome includes anticoagulation with thrombolysis or stenting, in specific circumstances. In those who do not respond to initial treatment, TIPS can be considered to decompress congested segments of the liver. In one large series TIPS placement was associated with similar five-year survival to liver transplantation for Budd-Chiari syndrome.
What are contraindications to TIPS?
Creation of a TIPS leads to a significant shift in blood volume from the splanchnic to the systemic circulation. This in turn increases venous return to the heart, right heart pressures and cardiac output. Therefore, absolute contraindications to TIPS placement include cardiac and pulmonary conditions that are likely to worsen with this significant increase in venous return to the right heart (Table 2).
Uncontrolled systemic infection is considered a contraindication to TIPS due to concern for TIPS seeding. Clinical circumstances of TIPS placement as well choice and timing of treatment for infection should determine the risk vs benefit of the procedure on a case-by-case basis.
Relative contraindications to TIPS include anatomic derangements that can reduce technical success or lead to complications. Following a discussion of risks and benefits and under the right clinical circumstances, TIPS can be successfully created by an experienced interventional radiologist despite these contraindications.
Table 2: Contraindications to TIPS.Table adapted from: Boyer TD and Haskal ZJ. The role of transjugular intrahepatic portosystemic shunt (TIPS) in the management of portal hypertension: update 2009. Hepatology 2010; 51(1): 306-322.
Hepatic encephalopathy is only a contraindication to TIPS when it cannot be controlled with medications. Careful case consideration and a discussion of risks and benefits should occur in patients with pre-existing hepatic encephalopathy, prior to TIPS placement.
What are the potential complications of TIPS?
Hepatic encephalopathy
Hepatic encephalopathy is a well-known complication of TIPS , particularly in the elderly, those who are sarcopenic, have alcohol-associated liver disease and those with pre-existing hepatic encephalopathy. The incidence of new or worsening hepatic encephalopathy following TIPS is 30-50%. Data on pharmacologic prophylaxis to prevent post-TIPS hepatic encephalopathy is somewhat mixed. Rifaximin prophylaxis is reasonable in patients at high risk for post-TIPS hepatic encephalopathy and has been shown to decrease rates of post-TIPS hepatic encephalopathy compared to placebo.Fortunately, in most patients, hepatic encephalopathy can be controlled with medications. TIPS occlusion to control encephalopathy is only required in 5% of patients.
Liver failure
Liver failure has been reported to occur in up to 20% of patients post-TIPS. TIPS creation involves the diversion of blood flow away from the portal vein and directly into the systemic circulation. This diversion creates an increase in hepatic artery flow in most patients. Patients who cannot increase arterial blood flow to the hepatic sinusoids are at risk for ischemic liver injury and liver failure. Proposed criteria for post-TIPS liver failure include 3x increase in total bilirubin or 2x increase in INR. Risk factors include MELD >18 and underlying cardiac disease.
TIPS dysfunction
TIPS dysfunction is defined as a loss of portal decompression with HVPG >12 mmHg or a recurrence of the portal hypertensive complication for which TIPS was placed. TIPS dysfunction can occur as a result of thrombosis or pseudo-intimal hyperplasia.
TIPS thrombosis most often occurs within the first month following placement. Thrombosis has been reported in 10-15% of patients with bare metal stents but data on covered stents is limited. Treatment options include thrombectomy, thrombolysis and anticoagulation. Prophylactic anticoagulation after TIPS placement is not routinely recommended.
Pseudo-intimal hyperplasia can lead to stenosis or occlusion of TIPS wherein the stent is coated with a collagenous matrix covered by endothelial cells.The routine use of polytetrafluoroethylene (PTFE)-covered stents rather than bare metal stents has decreased the incidence of stenosis and occlusion. One study estimated a 2-year patency of 76% in PTFE-covered stents vs 36% in bare metal stents.
TIPS placement is not a contraindication to liver transplant. The TIPS stent should extend as short a distance as possible into the portal vein and inferior vena cava to allow for creation of a durable stent without complicating anastomoses created during liver transplantation. Graft and patient outcomes are similar in those with and without pre-transplant TIPS.
Post-TIPS care
Following TIPS placement CBC, CMP and INR should be drawn within 72 hours to look for signs of bleeding and liver dysfunction. A baseline ultrasound with doppler should be performed within 3-7 days to assess patency with repeat ultrasounds at 1, 3 and 6 months following the procedure.Long-term surveillance includes ultrasound with doppler every 6 months with angiogram and HVPG measurement as necessary. The goal of surveillance is to detect TIPS stenosis prior to complete occlusion.
Diuretics should be resumed following TIPS placement at pre-TIPS doses with the goal of slowly tapering over 3-6 months.


