Peri-Procedural Management of Bleeding Risk in Cirrhosis
Procedural Risk
- Several classifications of bleeding risk associated with invasive procedures have been proposed.
- High risk procedures like major surgeries, interventional endoscopic procedures (endoscopy with polypectomy > 1 cm, submucosal dissection or mucosal resection, cystogastrostomy, percutaneous gastrostomy, endoscopic retrograde cholangiopancreatography with sphincterotomy, endoscopic ultrasound with fine needle aspiration etc.), solid organ biopsies, etc. have an estimated risk of major bleeding of 1.5% or more. Additionally, they are deemed high risk due to difficult to control bleeding, and significant morbidity and mortality that might arise even from minor bleeding occurring due to these procedures.
- Low risk procedures like transjugular liver biopsy are associated with bleeding risk that is easily detectable and controllable, which would include most vascular procedures (with the exclusion of transjugular intrahepatic portosystemic shunt [TIPS]) and local interventions (like dental extractions).
Coagulation and Hemostatic Parameters
INR
- INR is derived from the prothrombin time (PT), which reflects the activity of liver-derived clotting factors I, II, V, VII, and X. The term normalization refers to results being standardized among patients treated with vitamin K antagonists, like warfarin, to account for variation in the activity of proprietary thromboplastins – a key reagent in measuring PT. In patients with liver dysfunction, it is common to have prolongation of the PT and INR. PT/INR reflects only liver-derived procoagulant factors and does not account for significant deficiencies of liver-derived anticoagulant factors. As such, the INR alone is not a good measure of bleeding risk in patients with cirrhosis. Furthermore, because variceal bleeding in cirrhosis is pressure-driven from portal hypertension, efforts to correct the PT/INR with plasma may exacerbate portal hypertension, and thus prophylactic plasma transfusion is not recommended. Therefore, a target INR does not exist.
Platelets
- There is inconsistency between societal recommendations when it comes to thrombocytopenia in patients with cirrhosis undergoing invasive procedures.
- The American Association for the Study of Liver Disease (AASLD) abstain from a recommendation regarding routine preprocedural correction of thrombocytopenia before performing high risk of bleeding procedures due to lack of sufficient data.
- The Society for Interventional Radiology recommends a platelet count over 30 x 109/L as a safe threshold for performing high risk of bleeding procedures.
- The American Gastroenterological Association (AGA) and the American College of Gastroenterology (ACG) recommend a platelet count over 50 x 109/L as a safe threshold for performing high risk of bleeding procedures.
- At this point in time an individualized approach should be undertaken until definitive evidence is available.
Fibrinogen
- In patients with cirrhosis, plasma fibrinogen concentration levels < 100 mg/dL are associated with spontaneous and procedure-related bleeding. A caveat is that low fibrinogen levels may reflect critical illness and may not directly cause bleeding. There is lack of scientific evidence evaluating the efficacy of fibrinogen transfusion as procedural prophylaxis in patients with cirrhosis. Several societies and expert groups have recommended using cryoprecipitate (preferred over fresh frozen plasma due its large infusion volume) to replace fibrinogen in the setting of acute blood loss, with a goal fibrinogen level above 100-120 mg/dL. Of note, empiric correction of low fibrinogen is not recommended in patients who are neither bleeding nor undergoing invasive procedures.
TEG/Rotational Thromboelastometry (ROTEM)
- TEG and ROTEM measure the viscoelastic properties of a developing clot in a sample of whole blood, under low shear conditions. They provide real-time information about the quality of the clot and the kinetics of its formation.
- TEG and ROTEM have been shown to be helpful in transfusion management in patients with cirrhosis with non-variceal and variceal bleeding, and patients undergoing liver transplantation.
- TEG and ROTEM have been shown to decrease the need for prophylactic blood transfusions. However, these studies were not designed to determine if these tests can predict procedure-related bleeding. A prospective study showed that these tests were unable to predict liver biopsy-related bleeding. The limitation of this study was that they included patients with and without cirrhosis, as well as patients undergoing percutaneous and transjugular liver biopsy. At this point in time there are no clear recommendations for or against the use of TEG and ROTEM in this patient population.
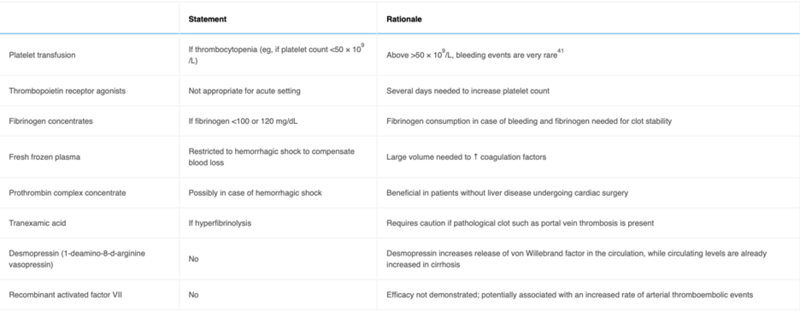
In addition, thrombocytopenia (if platelet count is below 50 x 109/L) and hypofibrinogenemia (if fibrinogen is below 100 mg/dL) should be corrected. Fresh frozen plasma and prothrombin complex concentrate should be restricted and can be considered in the setting of hemorrhagic shock.
Take Home Points:
- INR elevation due to chronic liver disease should not be corrected before an invasive procedure.
- There is lack of scientific evidence evaluating the efficacy of fibrinogen transfusion as procedural prophylaxis in patients with cirrhosis.
- Correction of thrombocytopenia is not necessary when platelet counts are above 50 x 109/L.
- It is reasonable to correct thrombocytopenia prior to an invasive procedure when platelet counts are below 50 or 30 x 109/L.
- You might be presented with challenging cases, like renal failure, systemic infections, severe anemia, and volume overload in addition to cirrhosis (compensated or decompensated). Recognize them and individualize patient care.