Management of Acute on Chronic Liver Failure in the Hospitalized Patient
What is Acute on Chronic Liver Failure (ACLF)?
Efforts to determine what constitutes “acute on chronic liver failure (ACLF)” have been ongoing in the literature since the early 2000s, when hepatologists saw the value in a common definition to unify research efforts and clinical care strategies. Due to the complex nature of advanced liver disease, there remains some debate as to which specific clinical factors should be included in the definition. Both the American Association for the Study of Liver Disease (AASLD) and the European Association for the Study of the Liver (EASL) working groups agree that there needs to be acute decompensation of chronic liver disease and at least one extrahepatic organ failure, but the details of the definitions differ in notable ways [see table 1].
| Table 1. Definitions of ACLF | ||
|
Society |
EASL-CLIF |
AASLD |
|
Similarities |
Acute decompensation of chronic liver disease. |
|
|
Differences |
|
|
How is this different from acute decompensated cirrhosis?
- Acute decompensated cirrhosis is a heterogenous syndrome characteristic of end-stage liver disease, while ACLF is the final and most fatal stage of acute decompensation of chronic liver disease and is characterized by massive systemic inflammation and multiorgan failure.
What Scoring Systems Help to Estimate Prognosis?
- CLIF-C ACLF score is useful when assessing patients in the critical care setting for consideration and listing for liver transplantation, early hospital discharge or determination of futility of ongoing intensive care unit supportive care in the absence of liver transplantation.
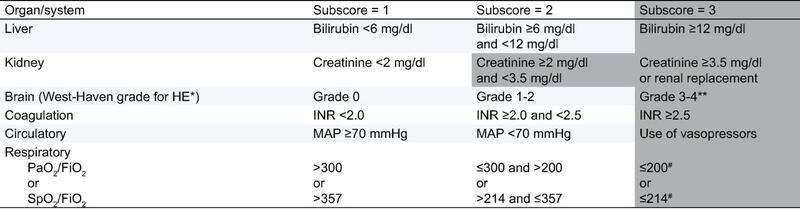
The CLIF-organ failure score system.
The shaded area describes criteria for diagnosing organ failures.
∗HE, hepatic encephalopathy; FiO2, fraction of inspired oxygen; PaO2, partial pressure of arterial oxygen; SpO2, pulse oximetric saturation.
∗∗Patients submitted to Mechanical Ventilation (MV) due to HE and not due to a respiratory failure were considered as presenting a cerebral failure (cerebral subscore=3).
#Other patients enrolled in the study with MV were considered as presenting a respiratory failure (respiratory subscore=3).
- Per the EASL-CLIF Consortium the worldwide mortality rate is 30-50%.
- The mortality rates in the Unites States per the North-American Consortium for the Study of End-Stage Liver Disease were 27%, 49%, 64%, and 77% with 1, 2, 3, and 4 organ failures, respectively.
- The 30-day readmission rate for patients discharged following an admission for ACLF is 30%.
How can we best care for patients with ACLF?
First: Treat the Precipitating Event
ACLF is often associated with a precipitating event, so workup to help uncover an underlying cause is an important first step in management. Common precipitating events include:
- Infection (bacterial, fungal) can be both a precipitating event but also a complication of ACLF. In hospitalized ACLF patients with evidence of ascites and unclear cause of presentation, diagnostic paracentesis should be obtained to rule out spontaneous bacterial peritonitis.
- See section on “infectious management below” for more details on workup.
- Gastrointestinal bleeding: acute variceal hemorrhage as well as other etiologies of GI bleeding are important causes of ACLF. In these cases, treatment includes a vasoconstrictor, antibiotic prophylaxis, and endoscopic therapy.
- Alcohol associated hepatitis: steroids are sometimes helpful in this scenario, however are not recommended in patients with ACLF-3 or in the presence of uncontrolled infection.
- Hepatitis B virus reactivation: this involves treatment with a nucleoside or nucleotide analogue.
Circulatory Support
Due to hyperdynamic circulation in decompensated cirrhosis, which leads to decreased vascular resistance, these patients have low arterial blood pressure and increased cardiac output. This pathophysiology worsens in patients with ACLF due to inflammation. Crystalloids and colloids can be the initial fluid of choice for patients who have hypovolemia.Albumin is recommended in HRS-AKI, spontaneous bacterial peritonitis, and large volume paracentesis.Norepinephrine is the first line vasopressor in ACLF.Relative adrenal insufficiency is common in critically ill patients. Diagnosis is based on adrenocorticotropin hormone stimulation test with cortisol levels. Lastly, an individualized mean arterial pressure target based on assessing adequacy of end-organ perfusion is preferable.
Hepatic Encephalopathy Management
Vigilant assessment of the airway and, if indicated, intubation (Glasgow coma scale ≤ 8 or HE grade III-IV) is important.Exclusion of other etiologies (intracranial hemorrhage, stroke, decompensated diabetes, psychiatric pathologies, alcohol associated dementia etc.) is necessary as well.Treatment of HE starts withlactulose 20g orally every hour until the first bowel movement and then titrated to maintain 2-3 soft bowel movements per day. Polyethylene glycol can be an alternative, especially in patients that are at risk of ileus/abdominal distension. The role of rifaximin in ACLF remains unclear currently.Renal replacement therapy has not been demonstrated to improve neurological outcomes in ACLF.Medications with short half-lives should be used for sedation and pain control.
- Withdrawal of diuretics and volume expansion with albumin (1 g albumin/kg of body weight, maximum 100 gm/day for 24-48 hours).
- Urine and imaging tests to determine the etiology of the renal injury.
- If the clinical picture is suggestive of HRS, a vasoconstrictor (terlipressin or norepinephrine) should be initiated.
- Renal replacement therapy can be a bridge to liver transplantation in those with reversible precipitant of their multiple organ failures, or in case of non-HRS-AKI.
Infectious Management

Coagulopathy
- Don’t use INR to gauge bleeding risk among patients with cirrhosis/ACLF.
- Viscoelastic testing (thromboelastography [TEG] and rotational thromboelastometry) provides a functional assessment of the altered pro- and anticoagulant pathways and measure platelet function, hyperfibrinolysis, and premature clot dissolution in real time. However, optimal cutoffs to guide blood products in ACLF have not been studied and this test is not widely available.
Nutrition and Supportive Care
- Oral feeding or enteral nutrition should be introduced early. A nasogastric tube for enteral feeding should be introduced in patients at high risk of aspiration. A nasogastric tube for enteral feeding is not contraindicated in patients with non-bleeding esophageal varices. After acute gastrointestinal hemorrhage it is recommended to withhold enteral tube placement for 48-72 hours.
- Monitoring for refeeding syndrome (e.g., hypokalemia, hypophosphatemia, arrythmias), especially in malnourished patients.
- Correction of electrolyte derangements.
Evaluation for Potential Liver Transplantation
- Early identification of patients who are eligible for liver transplantation is crucial since it can radically change patients’ prognosis. Thus, early referral to a liver transplant center is important!
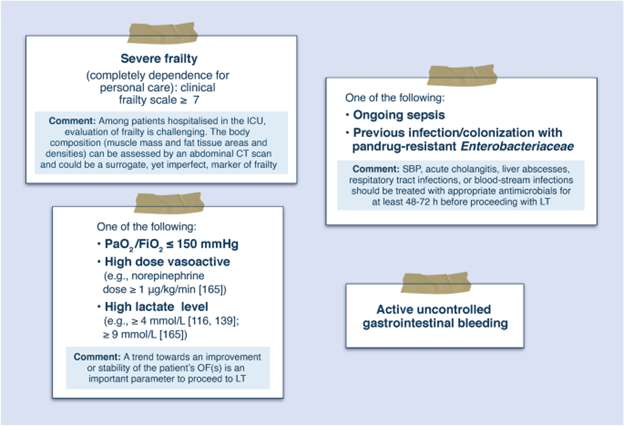
- Potential contraindications to liver transplantation include uncontrolled culture positive bacterial infection or uncontrolled infection for < 48 hours, refractory gastrointestinal bleeding despite TIPS, hemodynamic instability despite vasopressor support, respiratory failure with PaO2/FiO2 < 150, CLIF-SOFA score > 64 persisting for 3-7 days after ACLF diagnosis.
- If the patient is not a transplant candidate and has persistent organ failure after a brief period of support (48-72 hours), goals of care discussions and consultation with our palliative care colleagues is important due to the poor prognosis.
Back to the case
Due to his ACLF and no contraindications to transplant, he was listed for liver transplantation and discharged after 14 days with close follow-up and plan to complete an intensive outpatient program to assist him with alcohol cessation.
Take Home Points:
- ACLF is defined by AASLD as the presence of all of the following elements as minimum critical components: (1) acute onset with rapid deterioration in clinical condition, (2) the presence of liver failure defined by elevated bilirubin and elevated INR in patients with chronic liver disease with or without cirrhosis, and (3) the presence of at least one extrahepatic (neurologic, circulatory, respiratory, or renal) organ failure.
- Early identification of ACLF is important and management includes identification/treatment of the precipitating event, as well as cardiovascular stabilization, circulatory support, and airway protection.
- Other important factors in management of ACLF include treatment of HE, AKI, and low threshold for empiric antibiotics based on suspected source with adjustment for multidrug-resistant organisms if needed.
- Management of malnutrition with early enteral feeding is important.
- Due to the severity of illness and poor prognosis, early consideration of liver transplant at a liver transplant center is important, as well as early involvement of palliative care.