Steatotic Liver Disease: Cutting Through the Fat
Learning Objectives:
1. Understand the updated nomenclature of steatotic liver disease (SLD) and differentiate between its subcategories, including MASLD, ALD, MetALD, and cryptogenic SLD.
2. Evaluate current and emerging therapeutic strategies for MASLD, including lifestyle modifications, pharmacologic treatments, and novel investigational agents.
What is SLD?
Steatotic liver disease (SLD) is a broad term characterized by excessive liver fat accumulation. This is sub-classified into metabolic dysfunction-associated steatotic liver disease (MASLD), metabolic-alcohol-associated liver disease (MetALD), alcohol-associated liver disease (ALD), and cryptogenic SLD.
The most prevalent subtype, MASLD, was formerly known as non-alcoholic fatty liver disease (NAFLD). However, an international hepatology consensus redefined it in June 2023 to reflect its metabolic roots and eliminate exclusionary terminology. This change also introduced "metabolic dysfunction-associated steatohepatitis" (MASH) in place of non-alcoholic steatohepatitis (NASH), fostering a more precise, patient-centered, and nonjudgmental approach to disease classification.
ALD remains a distinct category driven by excessive alcohol consumption. At the same time, MetALD recognizes individuals with both metabolic dysfunction and moderate alcohol use, reflecting the complex interplay between lifestyle factors and liver pathology.
Diagnosing these conditions requires a comprehensive approach, incorporating clinical history, imaging modalities such as ultrasound, MRI, elastography, and biochemical markers. These updates aim to reduce stigma, enhance diagnostic clarity, and refine research efforts to develop targeted therapies for the growing global burden of steatotic liver diseases.
Other Causes of Steatotic Liver Diseases
| Category | Cause |
| Drug-Induced | Corticosteroids, Methotrexate, Amiodarone, Tamoxifen, Valproic Acid, Antiretrovirals (NRTIs) |
| Inherited/Genetic | Wilson’s Disease, Abetaliprotenemia, Glycogen storage disease, Lipodystrophies, Celiac disease |
| Nutritional | Total Parenteral Nutrition, Acute weight loss (post-bariatric surgery), Malnutrition |
| Viral | Chronic Hepatitis C (especially genotype 3) |
| Endocrine | PCOS, Hypopituitarism, Hypothyroidism |
Table 1: Other causes of steatotic liver diseases
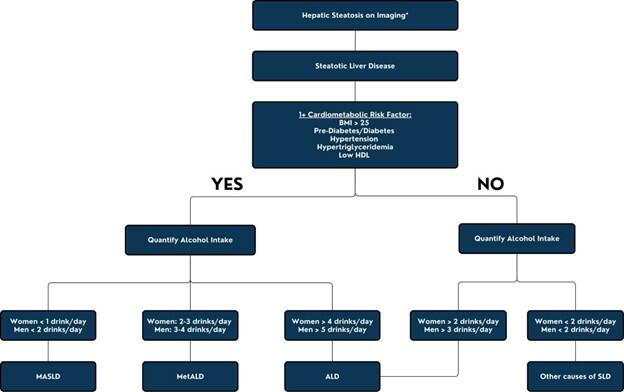
Figure 1: Differentiating SLD (Adapted from Israelsen et al)
*Imaging includes ultrasound, computed tomography, MRI, or elastography
Guideline-directed treatment for MASLD
Lifestyle Modifications:
- Weight Loss: Achieving a 5–10% weight reduction is associated with significant improvements in hepatic steatosis, inflammation, and fibrosis. Weight loss exceeding 10% has been linked to the resolution of steatohepatitis in up to 90% of patients.
- Dietary Changes: The adoption of a hypocaloric diet, particularly the Mediterranean diet rich in monounsaturated fats, has demonstrated efficacy in reducing liver fat content and improving insulin sensitivity.
- Physical Activity: Aerobic and resistance training exercises are recommended to decrease hepatic steatosis. High-intensity interval training (HIIT) may offer superior benefits compared to moderate-intensity continuous exercise. Resistance training can increase basal metabolic rate.
Pharmacologic Therapies:
| Medication | Mode of Action | Adverse Reaction |
| Pioglitazone | Activates PPARy, enhancing insulin sensitivity and reducing hepatic fat accumulation | Weight gain, edema |
| Vitamin E | Reduces oxidative stress and inflammation in the liver | Hemorrhagic stroke, prostate cancer risks |
| Improves insulin resistance, reduces hepatic lipogenesis, anti-inflammatory, weight loss, modulates lipid metabolism | Nausea, vomiting, diarrhea, pancreatitis | |
| Resmetirom* | Activates thyroid hormone receptor B, enhancing lipid metabolism and reducing hepatic fat | Nausea, vomiting, diarrhea, changes in thyroid hormone levels |
Table 2: Potential pharmacologic options for MASLD, with resmetirom* being the only current FDA-approved therapy
Management of Comorbid Conditions:
1. Cardiovascular Risk Factors:
Diligent management of hypertension, hyperlipidemia, and other cardiovascular risk factors is crucial, given the elevated risk of cardiovascular morbidity and mortality in MASLD patients. Statin therapy is also recommended based on the ASCVD risk score, and the risk of liver injury with statin use should not dissuade physicians from utilizing them if needed, as cardiac mortality risk is higher than hepatic mortality risk in patients with non-cirrhotic MASLD.
2. Diabetes Mellitus:
Optimal glycemic control is essential, utilizing agents that confer additional hepatic benefits, such as GLP-1 receptor agonists.
Bariatric Surgery:
For patients with a body mass index (BMI) >35 kg/m2 and MASLD, bariatric surgery can lead to significant weight loss and improvement in liver histology, including fibrosis regression. Surgical candidacy should be evaluated individually, considering potential risks and benefits.
Liver Transplantation:
In cases of decompensated cirrhosis or hepatocellular carcinoma secondary to MASLD, liver transplantation is a definitive treatment option. Post-transplant recurrence of MASLD is possible, necessitating ongoing management of metabolic risk factors and care coordination with primary care physicians and subspecialists.
The decision to perform bariatric surgery in the context of liver transplantation is complex and transplant center-specific. The AGA Clinical Practice Update on Bariatric Surgery in Cirrhosis suggests bariatric surgery as only viable concurrently or post-liver transplant. Bariatric surgery without liver transplant as a salvage or concurrent therapeutic option is contraindicated in patients with decompensated cirrhosis. There are clinical studies evaluating the role of combined sleeve gastrectomy with liver transplant in patients with MASLD, with some centers adopting this as part of their standard of practice.
Take-Home Points:
1. Non-alcoholic fatty liver disease (NAFLD) is now known as MASLD to better reflect the metabolic etiology of the condition and to remove stigmatizing language.
2. Management of MASLD focuses on lifestyle modifications, with a 5–10% weight loss improving liver fat accumulation, inflammation, and fibrosis. Resmetirom is the only current FDA-approved pharmacologic therapy for patients with F2-F3 fibrosis. There are several emerging therapies in the research pipeline.
3. Cardiovascular risk factors should be diligently managed, and statins should not be withheld for fear of hepatotoxicity.
