Bilirubin Pathways and Pitfalls: From Processing to Pathology
Bilirubin Pathways & Pitfalls: From Processing to Pathology
Learning Objectives:
- Review the physiology of bilirubin metabolism
- Differentiate between unconjugated from conjugated hyperbilirubinemia
- Recognize liver disease scoring systems and models that leverage bilirubin in liver dysfunction
How is bilirubin metabolism an essential function of the liver?
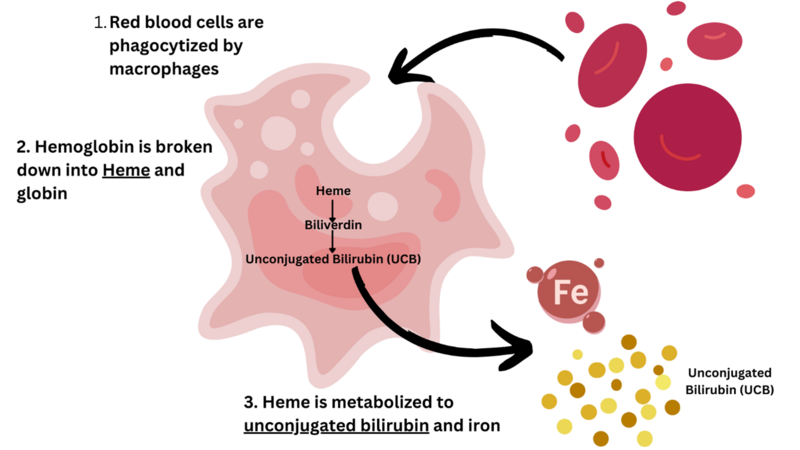
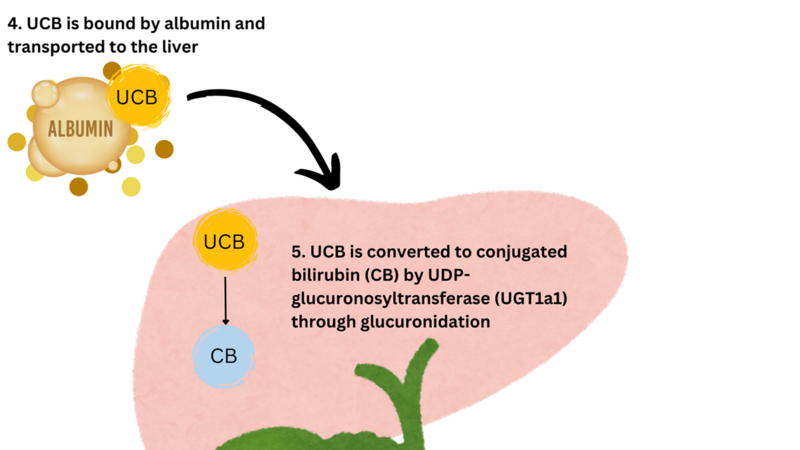
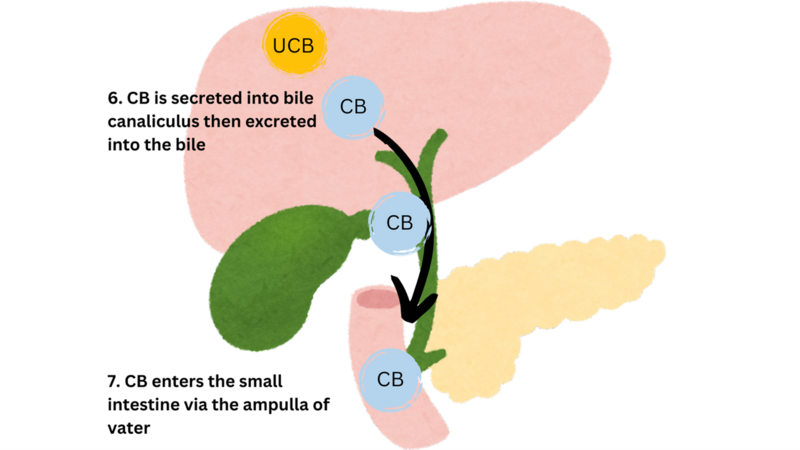
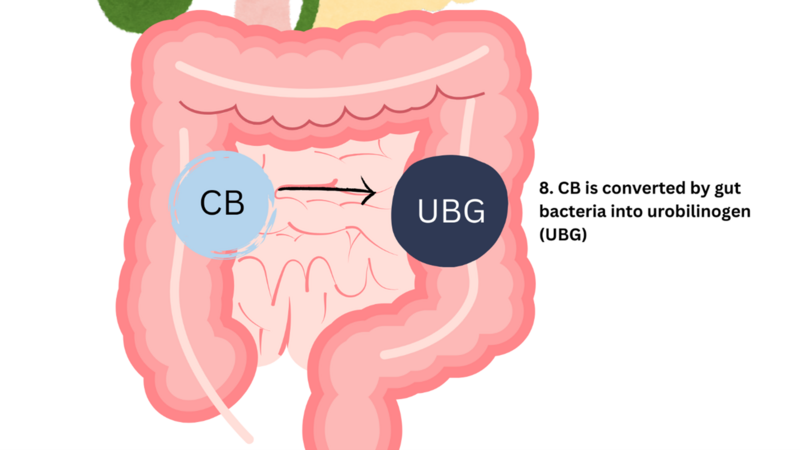
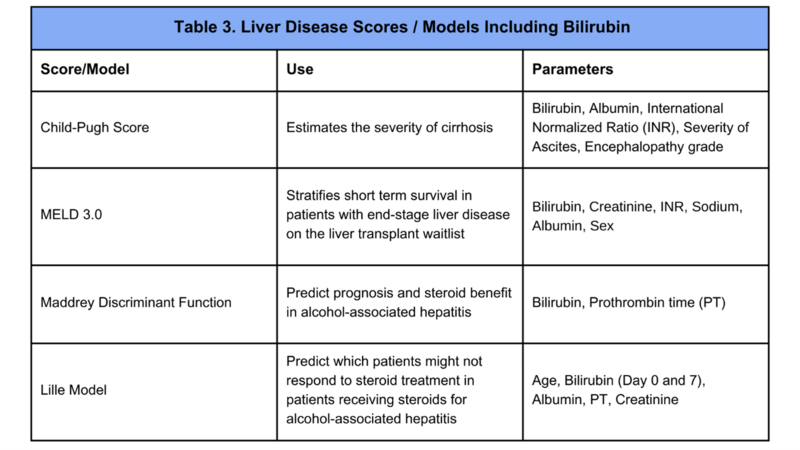
Bilirubin processing is a reflection of liver function, specifically the liver’s ability to clear metabolic waste. Understanding the basics of bilirubin metabolism (Figure 1) is essential to understand why jaundice occurs and to recognize liver pathophysiology.
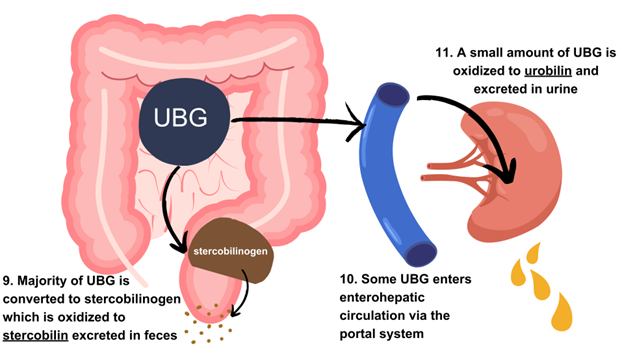
Figure 1. A Stepwise Overview of Bilirubin Metabolism
Figure created using Canva.com
Fast facts on bilirubin metabolism:
- About 70% of bilirubin is derived from catabolism of hemoglobin released from senescent red blood cells, 10% from ineffective erythropoiesis, and 20% from breakdown of heme-containing proteins in hepatocytes.
- Unconjugated bilirubin is hydrophobic and must bind albumin in plasma for transport to the liver. Low albumin levels impair bilirubin clearance by reducing the binding capacity and affinity for bilirubin, leading to reduced hepatic uptake.
- Conjugated bilirubin is hydrophilic which enables biliary excretion without transport.
What happens when bilirubin processing is impaired?
Hyperbilirubinemia occurs in the setting of bilirubin accumulation. The normal level for bilirubin in blood is <1 mg/dL. When bilirubin levels are >3 mg/dL, clinical features associated with hyperbilirubinemia can be appreciated. Jaundice, or yellow discoloration of the skin, sclera (scleral icterus), and mucous membranes, is the most common clinical feature of hyperbilirubinemia. Additional clinical features that can occur with pathologic accumulation of bilirubin include dark urine (due to increased urinary excretion of conjugated bilirubin) and pale (acholic) stools, with decreased bilirubin reaching the intestines.
What is the difference between Conjugated and Unconjugated Hyperbilirubinemia?
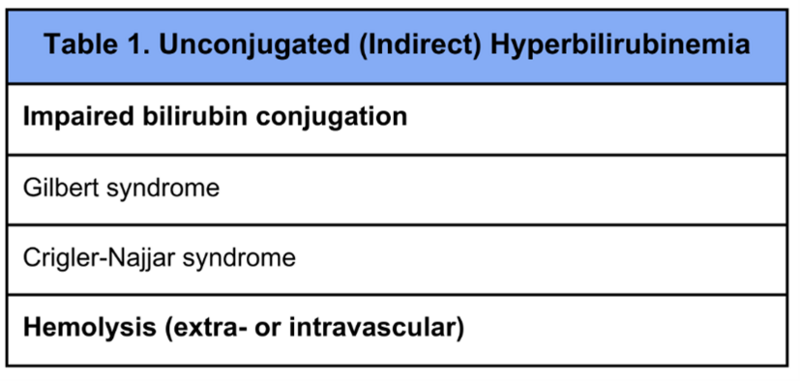
When bilirubin metabolism is altered, a variety of conditions can occur. Unconjugated (or indirect) hyperbilirubinemia occurs in the setting of both impaired hepatic bilirubin uptake and with increased heme turnover or hemolysis (Table 1). A key enzyme that catalyzes glucuronidation, conversion of unconjugated bilirubin to conjugated bilirubin, is uridine diphosphate-glucuronosyltransferase 1a1 (UGT1a1).
Gene mutations causing reduced enzyme activity level result in conditions in which there is an unconjugated hyperbilirubinemia. These include:
Gilbert syndrome is a benign hereditary condition resulting from mild reduction in UGT1a1 enzyme activity level (~30% gene activity). Gilbert syndrome is one of the most common etiologies of unconjugated hyperbilirubinemia and is estimated to affect approximately 3-7% of individuals. Patients with Gilbert syndrome are generally asymptomatic outside of jaundice which commonly occurs in the setting of stressors (i.e. dehydration, fasting, illness, or menstruation). In Gilbert syndrome elevation in serum bilirubin level is modest, usually less than 3 mg/dL. Diagnosis of Gilbert syndrome can be inferred based on lab findings of mild elevation in unconjugated bilirubin, clinical picture, and after ruling out active hemolysis and underlying liver disease. Confirmation of diagnosis through genetic testing for polymorphisms of the UGT1a1 gene is rarely pursued or of clinical utility as the condition is benign and self resolves with resolutions of stressors.
Crigler-Najjar syndrome is an inherited autosomal recessive condition resulting from moderate reduction (Type 2) or complete absence (Type 1) of the UGT1a1 enzyme. Unconjugated hyperbilirubinemia is present at birth, and patients have persistent elevation in the serum bilirubin ranging from 20-45 mg/dL in Crigler-Najjar type 1 and 5-25 mg/dL in Crigler-Najjar type 2.
Unconjugated hyperbilirubinemia is also seen with increased red blood cell turnover because the rate of heme metabolism and unconjugated bilirubin production exceeds the rate of conversion of unconjugated to conjugated bilirubin. Blood tests to evaluate for hemolysis include LDH, haptoglobin, reticulocyte count, and peripheral blood smear. Jaundice can occur in the setting of blood transfusion reactions with both intra- and extra-vascular hemolysis. Jaundice can also be observed in the setting of trauma with severe injury inducing intravascular hemolysis and increased lysis of both native red blood cell lysis and transfused red blood cells. Serum bilirubin levels rarely exceed 4-5 mg/dL in disorders related to hemolysis as patients tend to have normal liver function.
Conjugated hyperbilirubinemia occurs in the setting of both intrahepatic and extrahepatic cholestasis (Table 2). Intrahepatic cholestasis involves conditions that impair hepatic excretion of conjugated bilirubin into the bile canaliculi, with chronic liver disease such as cirrhosis being the most common cause. Extrahepatic cholestasis involves conditions where there is obstruction of bile ducts outside the liver, which prevents conjugated bilirubin from reaching the intestines. It is important to recognize that in cholestasis, bile acid transport is primarily impacted. While metabolism of bilirubin is mostly independent from bile acid metabolism, cholestasis impacts bile acid transport AND results in conjugated hyperbilirubinemia due to impaired hepatobiliary transport and transport protein function.
Dubin-Johnson and Rotor syndromes are rare, benign autosomal inherited disorders, resulting in conjugated hyperbilirubinemia. Conjugated bilirubin is excreted into bile via the multidrug resistance-associated protein 2 (MRP2) transporter. In Dubin-Johnson syndrome, impaired hepatic excretion of bilirubin occurs due to gene mutations resulting in impaired function of MRP2. The hallmark feature of Dubin-Johnson syndrome is the liver appearing black in the setting of impaired metabolite excretion. Some conjugated bilirubin enters hepatocytes from the bloodstream through re-uptake via organic anion-transporting polypeptides (OATPs). In Rotor syndrome, impaired hepatic uptake of bilirubin occurs due to gene mutations resulting in impaired function of OATPs. Outside of mild jaundice, patients with Dubin-Johnson and Rotor syndromes have normal liver function tests, absence of hemolysis, and are generally asymptomatic.
A stepwise approach to isolated hyperbilirubinemia can be reviewed in a previous Back to Basics post.
Bilirubin and Liver Dysfunction
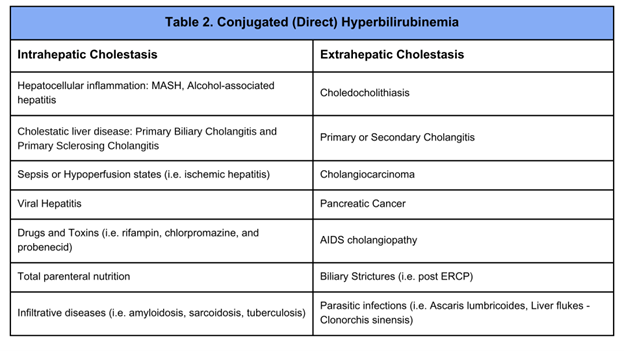
Elevated bilirubin can be an early warning signal of hepatic dysfunction. Several scoring systems and models (Table 3) have been developed for use in liver disease and leverage the role of bilirubin in the liver’s metabolism of waste products. These scores can be found on https://www.mdcalc.com/. In addition to abnormal coagulation factors, it is an important clinical clue to a patient’s synthetic dysfunction which can inform clinical decision making in a patient with advanced liver disease.
Take-home points:
- Bilirubin metabolism occurs in a series of steps following hemoglobin breakdown and results in the excretion of conjugated bilirubin as waste products, stercobilin and urobilin.
- Impaired bilirubin metabolism can occur in the setting of intrahepatic and extrahepatic cholestasis and result in both unconjugated and conjugated hyperbilirubinemia.
- Clinical features of hyperbilirubinemia include scleral icterus, jaundice, pale stools, and dark urine.
- Impaired bilirubin metabolism can be a reflection of liver disease and synthetic dysfunction, thus elevated bilirubin levels are a key component of commonly used scoring systems and models of liver disease.