ACLF: A Tipping Point in Chronic Liver Disease
ACLF: A Tipping Point in Chronic Liver Disease
Learning Objectives
- Identify and outline basic pathophysiology of acute on chronic liver failure (ACLF)
- Differentiate ACLF from acute liver failure (ALF) and acute decompensation of cirrhosis (AD)
- Discuss treatment considerations and recommendations for ACLF management
- ACLF refers to a clinical syndrome in patients with known cirrhosis or chronic liver disease who develop acute decompensation and multi-organ failure.
What is ACLF and how is it diagnosed?
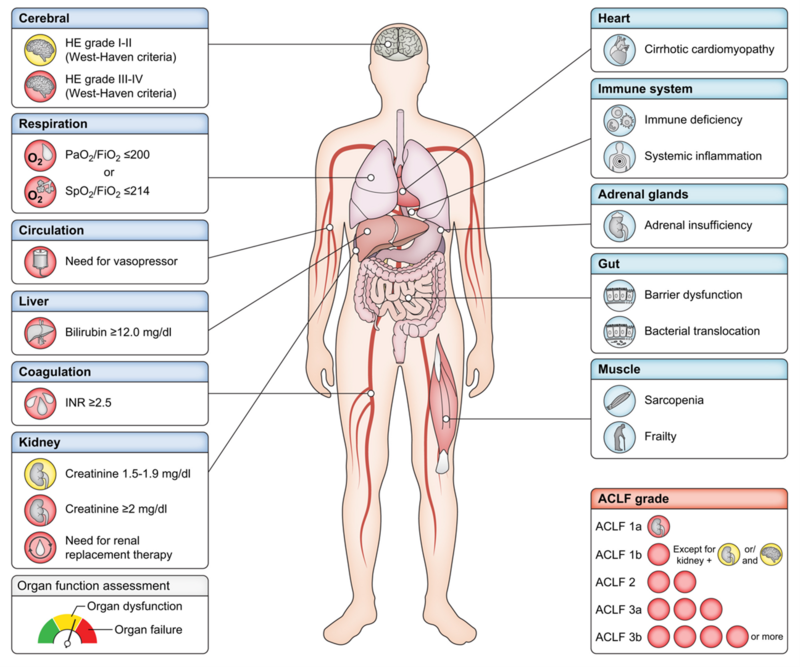
ACLF is a distinct clinical entity characterized by the onset of one or more hepatic and/or extrahepatic organ failures (OF) in patients with underlying chronic liver disease (CLD) who experience acute hepatic decompensation. Examples of AD include acute development of hepatic encephalopathy, gastrointestinal hemorrhage, ascites, or infection requiring hospitalization. International consortia, including the North American Consortia for the Study of End Stage Liver Disease (NACSELD), European Association for the Study of the Liver- Chronic Liver Failure (EASL-CLIF), and Asian Pacific Association for the Study of the Liver (APASL) have developed diagnostic criteria for ACLF with heterogeneity in defining ACLF patients and varying cutoffs for OF. Various parameters to consider in evaluation of OF for key organ systems, per EASL-CLIF, are outlined in Figure 1. ACLF severity is often stratified into 3 grades, with each grade corresponding to increasing number of organ failures and 28-day mortality, ranging from 22% in grade 1 patients to as high as 76% in grade 3 patients.
Figure 1: Organ Failure in ACLF per EASL-CLIF Consortium Criteria
Figure 1: The left side of the image depicts the six key organ systems used in CLIF organ failure scoring criteria (red and orange indicate organ failure and dysfunction, respectively) with additional organ systems that may be affected depicted in blue on the right. ACLF grading criteria is defined on the bottom right.
While the most common precipitating event in ACLF is infection, other precipitants include bleeding such as variceal bleed, alcohol-associated hepatitis (AH), acute hepatitis A or E infection, or hepatic ischemia. Of note, more than 40% of patients do not have an identifiable precipitating event and thus it is not required for diagnosis.
What are the underlying mechanisms that drive ACLF?
Patients with cirrhosis develop portal hypertension and enhanced gut permeability. This allows translocation of bacteria and/or pathogen-associated molecular patterns (PAMPs) from the intestinal lumen to intestinal mucosa, leading to local and systemic inflammation and chronic immune dysregulation, termed cirrhosis associated immune deficiency.
The systemic inflammation hypothesis posits that both ACLF and acute decompensated cirrhosis arise from inflammatory processes triggered by intestinal translocation or acute liver injury, such as acute alcohol-associated hepatitis, in cirrhotic patients with a baseline proinflammatory state. Prolonged inflammation and immune system hyperactivation can lead to reactive immune paralysis, also known as immune exhaustion, similar to patients with severe sepsis (Figure 2). Severe inflammation is also “energetically expensive” which can over time damage mitochondria and also contribute to OF.
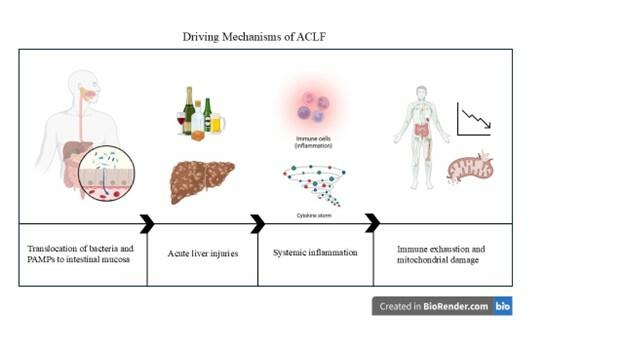
Figure 2: ACLF can be triggered by bacterial translocation or acute liver injuries, and with chronic systemic inflammation, leads to immune exhaustion and mitochondrial damage.
How does ACLF differ from acute liver failure and acute decompensation of cirrhosis?
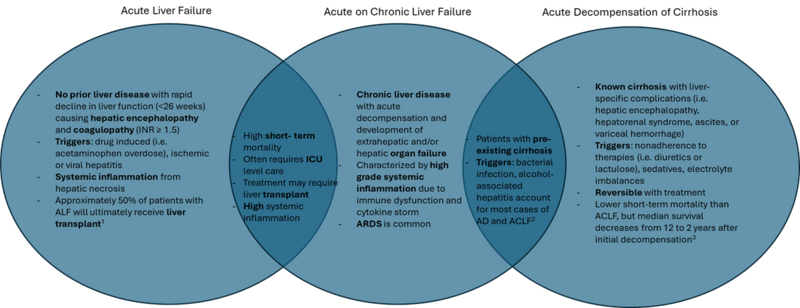
ACLF, ALF, and AD of cirrhosis are distinct clinical entities with unique clinical implications and management (Figure 3). By definition, ALF refers to patients without preexisting liver disease or cirrhosis who develop severe liver dysfunction with coagulopathy (INR ≥ 1.5) and hepatic encephalopathy. AD of cirrhosis on the other hand, refers to worsening liver function in patients with known cirrhosis resulting in hepatic encephalopathy, variceal hemorrhage, ascites, or hepatorenal syndrome. Finally, ACLF is triggered by acute hepatic insults in patients with chronic liver disease or cirrhosis and causes multi-organ failure in the setting of severe systemic inflammation. Of note, distinguishing ACLF from ALF if patient’s history of underlying cirrhosis is unknown can be challenging but is important given differences in treatment and overall prognosis.
Figure 3: Key differences between acute liver failure, acute on chronic liver failure, and acute decompensation of cirrhosis.
1: Acute Liver Failure Guidelines
2: Triggers for ACLF and AD
3: Median Survival Following AD
What are the principles of ACLF management?
ACLF is typically managed in the intensive care unit and inherently requires multidisciplinary collaboration between specialties such as hepatology, critical care, nephrology, and often palliative care. At this time, there are no targeted therapies, such as therapies to address systemic inflammation or immunoparesis, in ACLF. Management involves organ support (i.e. mechanical ventilation or renal replacement therapy for respiratory and renal failure, respectively), treatment of precipitating factors (i.e. infection), and increasingly, evaluation for liver transplantation in patients who have not become too sick from multiorgan failure. Accordingly, addressing the PIRO principles, which were initially developed for sepsis-related organ failure, can help guide management (Table 1).
Table 1: PIRO Principles Applied to ACLF
| PIRO Principle | Examples | |
| P | Predisposing factor (baseline risk factors) | Optimization of nutritional status, comorbid conditions |
| I | Injury (precipitant) | Management of GI bleed, alcohol-associated hepatitis, ischemic events |
| R | Response (inflammation or infection) | Management of systemic inflammation and cytokine storm, antibiotics to address bacterial infection |
| O | Organ support (intensive care) | Intubation for airway protection in HE, mechanical ventilation for respiratory support, renal replacement therapy, evaluation of liver transplant candidacy |
Take Home Points
- ACLF is a distinct clinical entity from both acute liver failure and decompensated cirrhosis, distinguished by multi-organ failure and poor prognosis.
- While there are no therapies specific to ACLF, management involves organ support, treatment of ACLF precipitant, and increasingly in cases without recovery, consideration of liver transplant evaluation.