Why (and how) does coagulopathy occur with liver disease? -- Part 1
We’ve all asked ourselves...is my cirrhotic patient going to bleed after this paracentesis? Why did they develop a blood clot with an INR of 2.5? Should I give them vitamin K or FFP before removing a polyp? In this multi-part series, I am going to try and summarize answers to all of these questions (and more) as we learn about the coagulopathy of liver disease.
My rough outline for the series is as follows: This first post will review normal hemostasis to introduce some important players and create a foundation moving forward.
Subsequent posts will address the following:
- Effect of cirrhosis on the components of hemostasis
- Overview of common tests to assess risk of bleeding or clotting and accuracy in liver disease
- Are there more reliable ways of measuring bleeding/clotting risk in cirrhosis?
- Clinical evidence of the actual risk of bleeding or clotting in cirrhosis
- Evidence for or against medical treatments and blood products in patients with cirrhosis
Ok, let’s get started.
The stages of hemostasis
I am going to discuss hemostasis in 4 distinct stages, as follows:
- Endothelial disruption
- Platelet aggregation/activation
- Coagulation cascade
- Fibrinolysis
For each stage, I’ll introduce to you some of the relevant players and then depict the important steps in clotting that occur within that stage.
Stage 1: Endothelial disruption
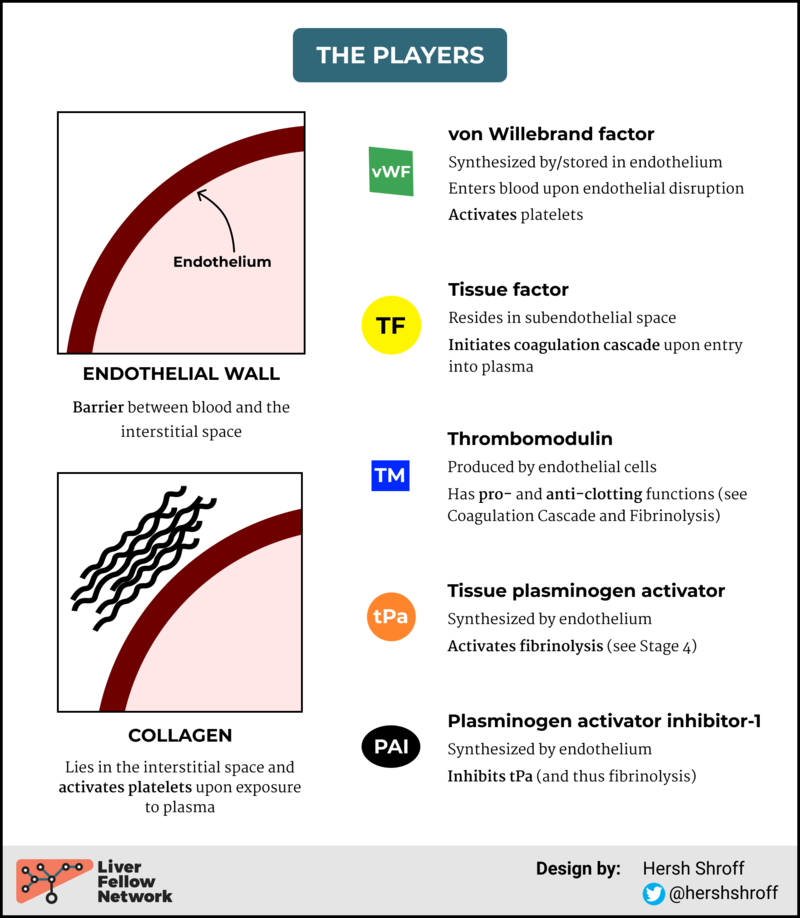
FIGURE 1: PLAYERS IN ENDOTHELIAL FUNCTION
Endothelial disruption is an important trigger for the hemostatic cascade. It occurs through direct trauma or injury, as well as with shear stress, hypoxemia, sepsis, and chronic inflammatory states (cirrhosis!). Here’s what happens as a result.
FIGURE 2: STEPS IN ENDOTHELIAL DISRUPTION
Stage 2: Platelet activation and aggregation
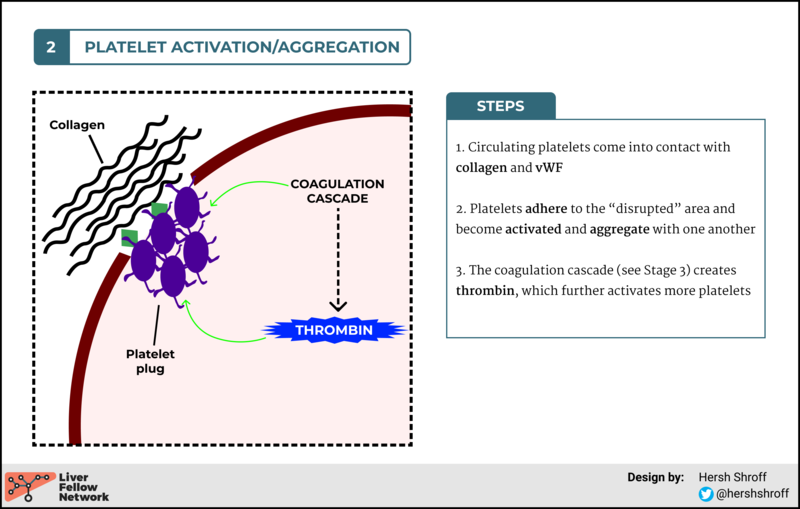
Our body’s first response to endothelial disruption is to try and “plug up the hole.” That’s where platelets enter the picture. There are three major steps to platelet plugging (see Figure 3):
- Adhesion (to the area of disruption)
- Aggregation (with other platelets)
- Providing a phospholipid surface on which coagulation cascade reactions can occur
FIGURE 3: STEPS IN PLATELET ACTIVATION AND AGGREGATION
For more details regarding platelet activation and aggregation, see here.
Onto Stage 3: The coagulation cascade…
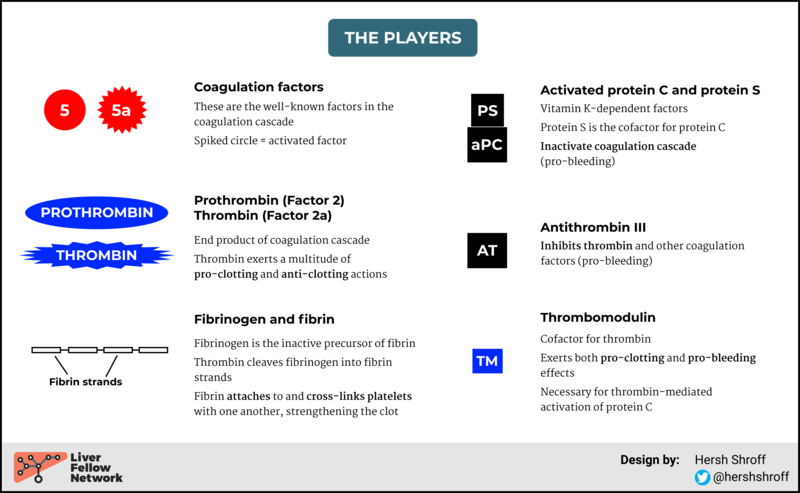
Let’s introduce a few new players.
FIGURE 4: COAGULATION CASCADE PLAYERS
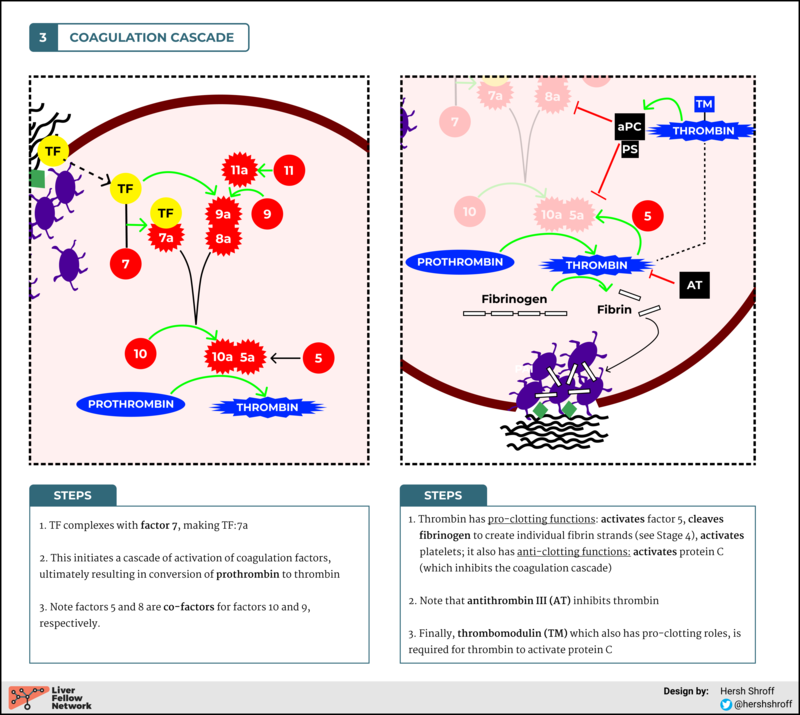
FIGURE 5: STEPS IN THE COAGULATION CASCADE
Make a note of the importance of thrombin. It regulates the entire process, exerting both “pro-clotting” and “pro-bleeding” effects. Ultimately, it is the key output of the complex coagulation cascade. As we will discuss in later posts, the ability to generate thrombin (i.e. the endogenous thrombin potential or ETP) is an important way to measure clotting ability and may provide a more global picture than studying perturbations in individual components of the cascade.
Also just to highlight some players in the negative feedback process (see here for more):
- Protein C and Protein S -- vitamin K dependent anti-clotting factors, formed in the liver, inactivate factors 5a and 8a
- Antithrombin III (ATIII) -- inhibits thrombin and many other coagulation factors
- Tissue factor pathway inhibitor (TFPI) -- not to be confused with TAFI. TFPI binds to and inhibits the factor 10a:5a complex as well as the TF:7a complex
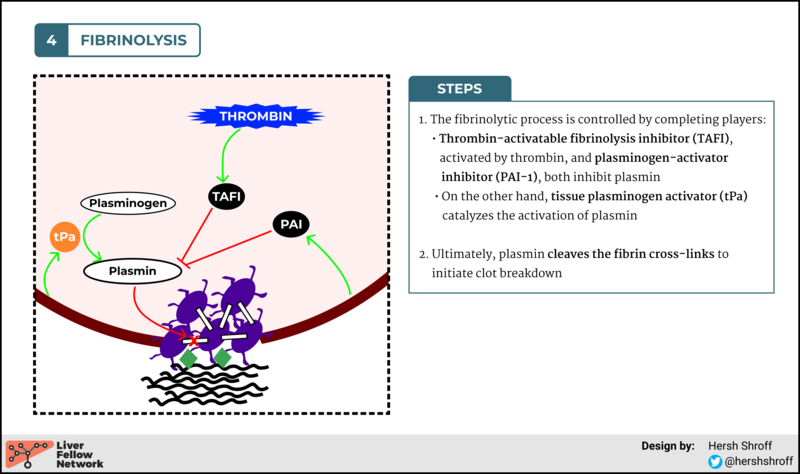
Stage 4: Fibrinolysis
Fibrinolysis is the final stage, occurring after vascular integrity has been restored, with the intent of breaking down the clot and restoring a normal vasculature.
The only new player here is plasmin (with its inactive precursor, plasminogen).
- Plasmin’s major role is to bind to and cleave fibrin, thus initiating fibrinolysis
- Plasmin also has positive auto-feedback (activates more plasminogen into plasmin)
FIGURE 6: STEPS IN FIBRINOLYSIS
...and that’s it!!
Now that we have a foundation of the normal hemostatic mechanisms, stay tuned for my next post discussing how these are affected by end-stage liver disease!
Other References
- Colman RW, Clowes AW, George JN, et al. Chapter 1: Overview of Hemostasis. In: Colman RW, Clowes AW, Goldhaber SZ, Marder VJ, George JN, eds. Hemostasis and Thrombosis: Basic Principles and Clinical Practice. 5th ed. Lippincott Williams & Wilkins 2006.
- DeLoughery T.G. (2015) Basics of Coagulation. In: DeLoughery T. (eds) Hemostasis and Thrombosis. Springer, Cham. https://doi-org.ezproxy.galter.northwestern.edu/10.1007/978-3-319-09312-3_1.