Why do we use non-selective beta-blockers in cirrhosis? - Part 2
At the end of Part 1 of this series, I discussed the Groszmann NEJM study -- a negative trial using NSBBs to prevent the formation of varices. I also introduced the concept of clinically-significant portal hypertension (CSPH).
It was this crucial knowledge from prior studies that led to the design of a new trial, called PREDESCI, which is how we'll start Part 2.
What's the PREDESCI trial?
Remember how the Grozsmann trial included patients with very early portal hypertension (HVPG 6-10mmHg)? The PREDESCI trial focused only on patients with CSPH as the target population and chose decompensation as the outcome!
The investigators included patients with CSPH with no or small varices. The reason they did not include patients with medium/large varices is of course that these patients would have needed primary prophylaxis (per guidelines), so it would have been unethical to randomize them to placebo.
In this study, CSPH was identified via HVPG measurements and the response to NSBBs was evaluated by acute drop in HVPG >10% twenty minutes after the intravenous propranolol was administered. Responders were randomized to propranolol vs placebo, and propranolol non-responders were randomized to carvedilol vs. placebo. The primary outcome was decompensation or death.
And results were very impressive! The figure below demonstrates the cumulative incidence of decompensation or death during follow-up -- it was significantly lower in the NSBB group than in the placebo group (HR 0.51, 95% CI 0.26–0.97). The difference was mainly due to a difference in appearance of ascites, with 20% in the placebo group and 9% in the NSBB group (HR: 0.42 CI 0.19 – 0.92).

This landmark study was able to show a new indication for NSBBs, which is the prevention of decompensation in patients with CSPH even without medium or large varices. The study shows that this population also benefits from NSBBs.
The study suggests that patients with compensated cirrhosis should be screened for development of CSPH and treated with NSBBs to prevent decompensation and death. However, there are limitations to the study in terms of generalizability to clinical practice. In clinical practice, we use non-invasive tests instead of HVPG to identify patients with CSPH. The majority of the study subjects had alcohol and hepatitis C cirrhosis, so it is unclear at this point whether these findings are going to be similar in the growing population of NASH cirrhosis patients. And last but not least, we are not able to differentiate responders vs non-responders in clinical practice as we don’t measure HVPG while administering NSBBs!
Why is it important to identify the response to NSBBs?
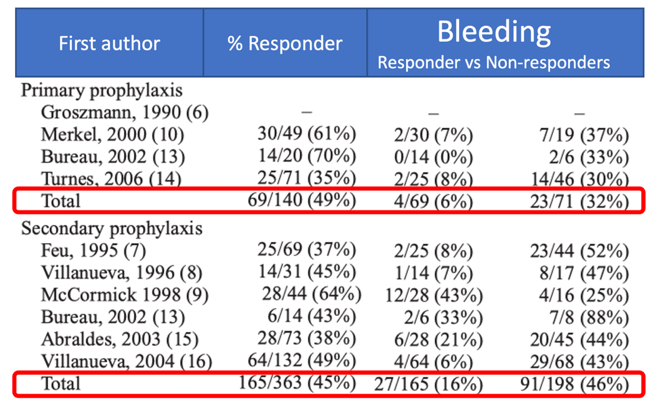
A meta-analysis of studies using NSBBs for primary and secondary prophylaxis with repeat HVPG measurements showed that the clinical benefits of NSBBs (such as improvement in survival and prevention of variceal bleeding) are mainly observed in responders (patients who have a reduction of HVPG by 20% or to less than 12). However, only about 50% of patients receiving traditional NSBBs (propranolol and nadolol) are responders. Here is a modified table from this meta-analysis, showing the risk of variceal bleeding is much higher in the non-responder group compared to responders.
The number of responders increases in patients receiving carvedilol. This is a graph from a study by Reiberger et al, showing that among propranolol non-responders, 57% achieved hemodynamic response when using carvedilol.

Although we do our best to identify responders and titrate the beta-blocker to achieve a HR goal of <60, it is important to remember that HR by itself is a poor marker for differentiating responders from non-responders. In a study by Abraldes et al., looking at long-term prognosis of NSBB responders vs non-responders (assessed by repeated HVPG measurement), non-responders still achieved the goal HR and there was no statistically significant difference in the overall HR between the two groups.
Why you might be nervous about using NSBBs? How do you choose the right patient population?
It's only fair to also talk about the disadvantages of NSBBs before making a decision. Patients might have absolute or relative contraindications to NSBB therapy, such as a heart block, uncontrolled asthma, or hypotension (SBP<90).
Patients also might not be able to tolerate the target dose or may discontinue the medication due to side effects. In a Cochrane review comparing NSBBs to band ligation for primary prophylaxis of variceal bleeding, NSBBs were associated with significantly more lethargy, dizziness, hypotension and impotence. Band ligation was associated with transient dysphagia/retrosternal pain and post banding bleeding complications.
Below is a graph from the Cochrane review focusing on the hypotension side effect. You can see the full set of comparison between different adverse events here.

It is essential to discuss the side effects and benefits of each treatment option with the patient and involve them in shared decision-making. In a small pilot study asking patients about their preferences in terms of EVL vs NSBB after explaining both alternatives, 64% of patients chose EVL. The caveat is that this was an older study and the potential benefits of NSBBs in prevention of decompensation were not included in the script that was used to educate the patients.
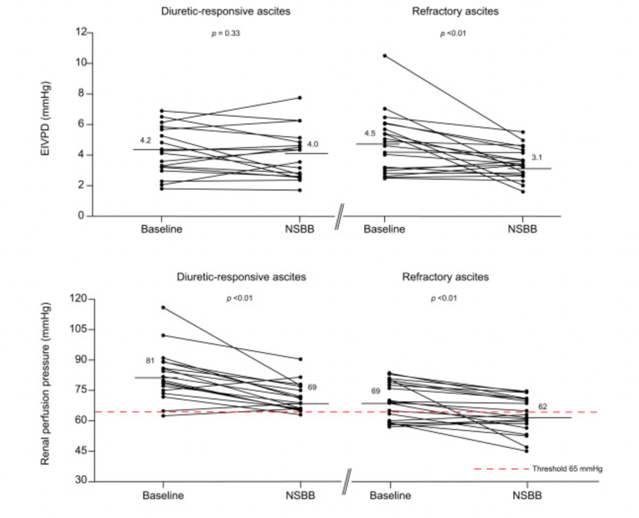
One of the very controversial topics is the use of NSBBs in patients with ascites (especially refractory ascites), as it can decrease renal perfusion and systolic function. Here is a graph from a study by Tellez et al, showing the changes in renal perfusion pressure and systolic function, 4 weeks after starting NSBBs.
On the other hand, multiple meta-analyses have shown an overall mortality benefit in subgroup analyses in patients with ascites or even refractory ascites. The controversy continues, but in my opinion a study by Tergast et al sheds some light into this. Below is a figure from the study showing LTx-free survival in patients with ascites. The top portion (B) consists of patients with MAP < 65mmHg, in whom NSBB therapy does not offer a benefit. The bottom portion of the figure (C), includes patients with MAP >= 65mmHg. In these patients, NSBB therapy led to statistically higher rate of LT-free survival.
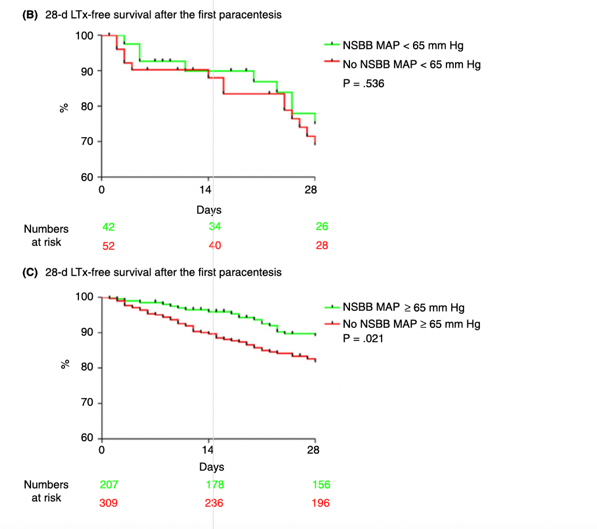
The study concludes that the systemic arterial blood pressure determines the therapeutic window of NSBBs in patients with decompensated cirrhosis. The key is to start at a lower dose, titrate carefully while the SBP is >90 and MAP is >65. It is important to note that carvedilol is not recommended in patients with ascites.
The controversy continues, and if you are interested in reading more about it, I urge you to take a look at the tweetorial by Elliot Tapper on this!
Now back to our patient from Part 1
A 54-year-old patient with compensated alcohol-associated cirrhosis with a liver stiffness measurement of 26 kPa and a platelet count of 145, endoscopy showing 2 columns of large varices with red wale markings. What would you do?
- Start a NSBB and not even send for EGD, as the patient already has CSPH based on non-invasive tests
- Send for EGD, but don’t do EVL, and after seeing the varices start them on NSBBs
- Send for EGD and do EVL
The correct answer might depend on who you ask (assuming that the patient does not have any contraindication to either option and has no specific preference in terms of therapy selection).
In my opinion number 1 is very progressive, and hopefully will be the future as more studies confirm the PREDESCI trial findings in the real-world practice setting.
Number 2 is my answer, based on current evidence.
I’m not a fan of option 3, however there are benefits to this option as well! With variceal ligation, we are able to see eradication, whereas with NSBBs we can’t easily identify the responders as we usually don’t measure HVPG in clinical practice. The other caveat is the difference between a randomized trial setting vs real world practice. Patients might be non-compliant with taking a daily medication, might not tolerate it, and titration to goal HR requires careful monitoring which could be challenging in the real world setting (in most trials, patients were seen every 3-4 days until they reached the HR goal).
I hope you enjoyed reading my 2-part series on beta-blocker therapy in cirrhosis. To end, I will leave you with some fun facts:
Red Wale: longitudinal dilated venules resembling whip marks on the variceal surface. It is not Vale and not Whale! It gets its name from the textile industry, the width of the cord in corduroy is commonly referred to as the size of the "wale" (i.e. the number of ridges per inch). The sign indicates the risk of future bleeding in a varix and it is NOT an indication that the varix has bled.
White nipple Sign: It is a platelet-fibrin plug at the site of the recent bleeding, and is a stigma of recent variceal hemorrhage. NEVER attempt to dislodge the lesion, and these varices need to be treated with EVL.
