Spare Me the Jab: Noninvasive Assessment of Patients with MASLD
1. Why is it important to establish liver disease severity?
- Patients with MASLD have increased overall mortality compared to patients without MASLD.
- There is growing evidence that patients with MASH and increased fibrosis are at higher risk of cirrhosis and liver-related mortality.
Back to the case
In the clinical case above, you recommend laboratory evaluation, which shows a platelet count of 203, AST 62, and ALT 72 (evaluation for alternate causes of abnormal ALT was unrevealing, and her abnormal ALT was attributed to MASLD). You calculate FIB-4, which is 1.51 points.
2. Primary risk assessment of patients with fatty liver disease
- You should start with a serologic test (e.g., fibrosis-4 index or FIB-4) with a high negative predictive value (NPV) to exclude advanced fibrosis. Although several tools exist including the NAFLD Fibrosis Score (NFS) and the AST to Platelet Ratio Index, FIB-4 is the most well-validated.
- FIB-4 has been recognized by the American Association for the Study of Liver Disease (AASLD) as a useful tool in identifying patients with higher likelihood of advanced liver fibrosis (F3 or F4). It is easily calculated using a patient’s age, AST and ALT level, and platelets.
- Patients with FIB-4 less than 1.3 can be safely followed in the primary care setting. They should be reassessed every 1-2 years if they have a diagnosis of diabetes type 2 (DMT2), pre-diabetes, or two or more metabolic risk factors (higher BMI, large waist size, high blood pressure, dyslipidemia). Patients should be reassessed every 2-3 years if they lack diagnosis of DMT2 and have less than two metabolic risk factors (see Figure 1).
- Patient with FIB-4 of 1.3 or greater should undergo secondary risk assessment. In patients with a FIB-4 score of greater than 2.67, advanced fibrosis is likely, though it is reasonable to still further assess with subsequent non-invasive testing for confirmation.
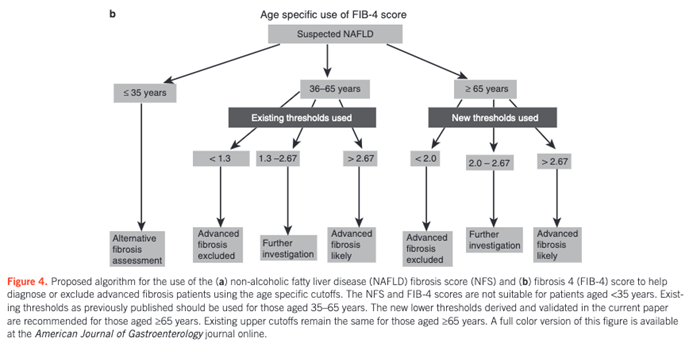
- FIB-4 is less reliable in patients under the age of 35 or over the age of 65. Patients who are 35 years or younger should have an additional alternative fibrosis assessment like vibration-controlled transient elastography (VCTE). Patients 65 years or older may be assessed with FIB-4 using different thresholds. If FIB-4 is < 2.0, advanced fibrosis is unlikely, and if it is between 2.0 and 2.67, further evaluation with alternative NIT is needed, and the threshold for likely advanced fibrosis (> 2.67) remains the same.
Back to the case
Because her FIB-4 was greater than 1.3, your patient underwent VCTE as part of her secondary risk assessment. This test showed liver stiffness measurement of 12.5 kPa.
3. What tool/s can you use for secondary risk assessment of patients with fatty liver disease?
- VCTE or Enhanced Liver Fibrosis (ELF) are the preferred tools for secondary risk assessment of patients with MASLD in the primary care or endocrinology practice settings.
- VCTE evaluates both fibrosis (liver stiffness expressed in kPa correlates with fibrosis) and steatosis (Controlled Attenuation Parameter [CAP] expressed in dB/m correlates with steatosis).
- The CAP score ranges from 100 to 400 dB/m. The CAP score categorizes the patient into a certain steatosis grade and the range of percentage of fatty changes:
- 238-260 dB/m=Steatosis Grade 1 [S1] =11-33% of the liver is with fatty change
- 260-290 dB/m=S2=34-66% of the liver is with fatty change
- higher than 290 dB/m=S3=67% or more of the liver is with fatty change
- The CAP score ranges from 100 to 400 dB/m. The CAP score categorizes the patient into a certain steatosis grade and the range of percentage of fatty changes:
- ELF is a commercial blood test that has been validated for identification of advanced fibrosis in patients with MASLD. It can be particularly helpful for patients who either do not have convenient access to a center with VCTE, have significant central adiposity that interferes with VCTE measurements, or have a cardiac device that is not approved for use with VCTE.
- Patients stratified to the low-risk group with the help of VCTE (< 8 kPa) or ELF (< 7.7) can be safely followed and reassessed in the primary care setting.
- Patients stratified to the intermediate risk group or high-risk group with the help of VCTE (8-12 kPa or >12 kPa, respectively) or ELF (7.7-9.8 or >9.8, respectively) may be considered for additional risk stratification with magnetic resonance imaging (MRI) based tests, if clinical uncertainty exists.
4. When to consider a liver biopsy?
- For patients designated to the intermediate/high-risk group based on NIT but with a high suspicion of cirrhosis, liver biopsy should be considered.
- In patients with indeterminate NIT, liver biopsy should be considered.
- In patients with diagnostic uncertainty (possible concomitant diagnoses), liver biopsy should be considered.
- In patients with persistently elevated ALT and AST (> 6 months), liver biopsy should be considered.
Figure 1. Algorithm for the Evaluation of Patients at Risk for or with Established NAFLD Across Practice Settings.
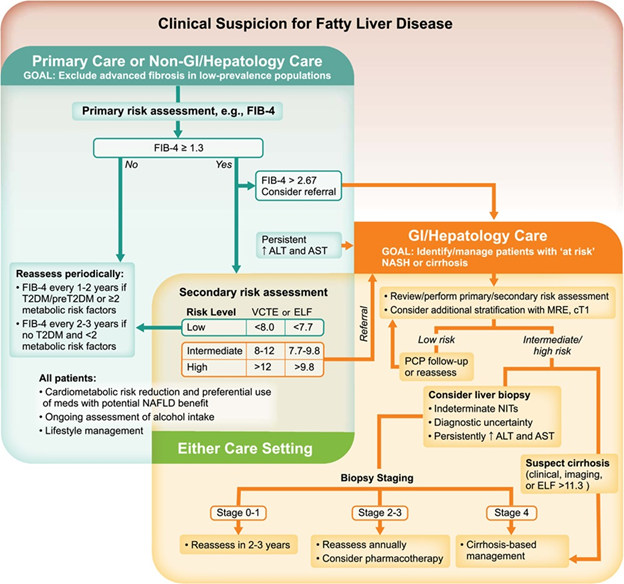
Figure from Rinella et al. Clinical Assessment and Management of Nonalcoholic Fatty Liver Disease: Practice Guidance from the American Association for the Study of Liver Diseases.
Take Home Points:
- In patients with suspected MASLD, NIT can be used in clinical practice for primary and secondary risk stratification.
- FIB-4 is well-validated and easily accessible in multiple practice settings. FIB-4 is a great tool to exclude advanced fibrosis and to monitor patients with ongoing risk of MASH and cirrhosis.
- For patients with FIB-4 >1.3 that are 36-65 years old and patients with FIB-4 >2 that are older than 65, VCTE or ELF should be used for secondary risk assessment to further risk stratify liver disease severity.
- MRI-based tests can be used to further risk stratify patients with indeterminate NIT or NIT that does not correlate with your clinical suspicion.
- Liver biopsy may be considered in patients with high clinical suspicion of cirrhosis, patients with indeterminate NIT, patients with diagnostic uncertainty, and patients with persistently elevated ALT and AST.
