Patterns of Cirrhosis
This edition of Pathology Pearls will focus on three major patterns of cirrhosis and the subtle histologic clues to the possible etiology. Grossly, there is a distinction based on the size of the nodules (<3 mm = micronodular, and >3 mm = macronodular). On the pattern of cirrhosis alone, you will be able to arrive at some possible etiologies for each.
Case #1: Centrilobular sinusoidal fibrosis: cirrhosis due to steatohepatitis
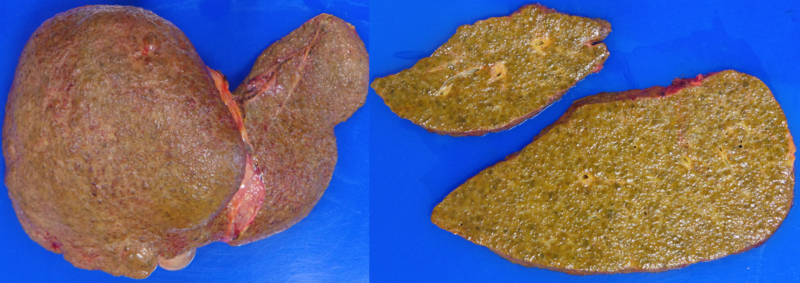
The patient is a 45-year-old with a history of alcohol-related cirrhosis complicated by decompensation with ascites and is undergoing liver transplantation.
| Liver enzymes | |
| AST | 71 U/L |
| ALT | 232 U/L |
| ALKP | 288 U/L |
| TBILI | 9.8 mg/dL |
| ALBUMIN | 2.9 g/dL |
Liver explant:
Alcoholic cirrhosis – micronodular surface appreciated on surface and cut section. Greenish color attributable to cholestasis with ongoing steatohepatitis.
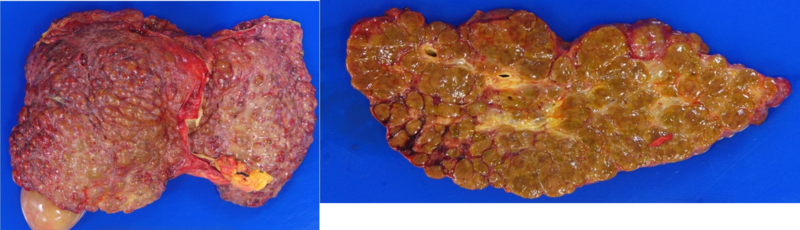
A) H&E, low power magnification – micronodular cirrhosis with macroregenerative nodule.
B) Trichrome, low power magnification – micronodular cirrhosis with macrovesicular steatosis.
C) Trichrome, medium power magnification – bands of fibrosis encircling small nodules of hepatocytes, ductular reaction as is expected with cirrhosis.
D) H&E, medium power magnification – cirrhosis with cholestatic steatohepatitis.
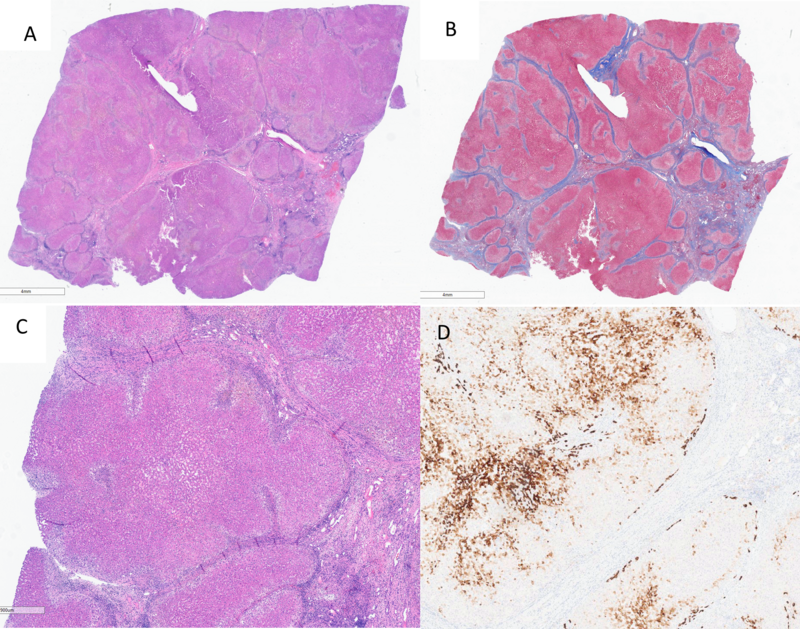
E) Trichrome, medium power magnification – fibrous obliteration of central veins, pericellular/sinusoidal fibrosis.
F) H&E, medium power magnification – prominent ballooning of hepatocytes (right), and cholestasis.
Key points: Cirrhosis due to steatohepatitis.
1. Clinical history – alcohol use, and/or metabolic dysfunction-associated steatotic liver disease (MASLD) (obesity, hyperlipidemia, diabetes).
2. Histology:
a. Steatohepatitis – steatosis, hepatocyte ballooning (+/- Mallory-Denk bodies), lobular necroinflammatory activity.
b. Fibrosis – centrilobular-sinusoidal fibrosis progressing to micronodular cirrhosis over time.
i. Fibrous obliteration of central veins more specific to alcohol use.
c. Steatohepatitis may be “burnt-out” meaning there has been cessation/improvement of the initial insult (improved diet or cessation of alcohol). There will be less steatosis and minimal ballooning of hepatocytes, or lobular necroinflammatory activity. Regression of fibrosis may also be seen.
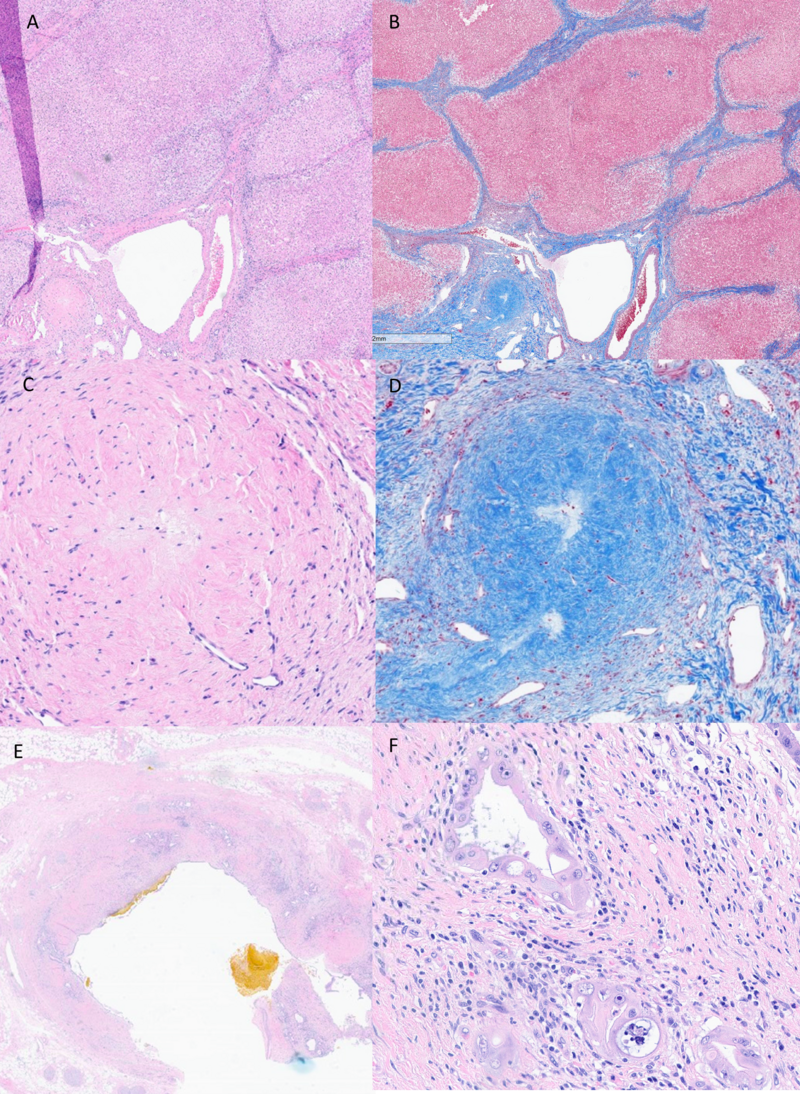
Case #2: Portal fibrosis: biliary cirrhosis
The patient is a 43-year-old patient with a history of PBC (AMA+, ANA+) with cirrhosis complicated by portal hypertension, gastropathy, esophageal varices, and hepatic encephalopathy, and is undergoing liver transplantation.
| Liver enzymes | |
| AST | 37 U/L |
| ALT | 8 U/L |
| ALKP | 159 U/L |
| TBILI | 3.8 mg/dL |
| ALBUMIN | 3.3 g/dL |
Liver explant:
Primary biliary cirrhosis (PBC) – biliary cirrhosis – macronodular cirrhosis on surface and cut section.
A) H&E, lower power magnification – macronodular cirrhosis.
B) Trichrome, low power magnification – macronodular cirrhosis with “jigsaw” fibrosis.
C) H&E, medium power magnification – macronodular cirrhosis with cholatestasis.
D) CK7 immunostain – loss of intrahepatic bile ducts and prominent hepatocyte biliary metaplasia.
Key points: Cirrhosis due to PBC.
1. Clinical history – middle aged (F>M), positive AMA serology, elevated IgM, elevated alkaline phosphatase.
2. Histology:
a. Florid duct lesion – seen early on, may also see granulomas.
b. Lymphocytic cholangitis -> periportal hepatitis.
c. Fibrosis – portal-based process with progression to macronodular “jigsaw” fibrosis.
d. Loss of intrahepatic bile ducts over time – hepatocyte biliary metaplasia (CK7 immunostain).
e. Cholatestasis - Chronic cholestasis leads to cholatestasis - feathery degeneration of periportal hepatocytes with enlarged, swollen with clear/granular cytoplasm.
Case #3: Portal fibrosis: biliary cirrhosis.
The patient is a 50-year-old with a history of primary sclerosing cholangitis-associated cirrhosis, as well as inflammatory bowel disease on therapy. The patient’s clinical course has been complicated by multiple decompensation episodes (including variceal bleed & portal vein thrombosis). The patient is undergoing liver transplantation.
| Liver enzymes | |
| AST | 471 U/L |
| ALT | 289 U/L |
| ALKP | 137 U/L |
| TBILI | 6.1 mg/dL |
| ALBUMIN | 2.9 g/dL |
Liver explant:
Primary sclerosing cholangitis (PSC) - biliary cirrhosis – macronodular cirrhosis on surface and cut section.
A) H&E, lower power magnification – macronodular cirrhosis.
B) Trichrome, low power magnification – macronodular cirrhosis with “jigsaw” fibrosis.
C) H&E, medium power magnification – fibro-obliterative lesion of PSC.
D) Trichrome, medium power magnification – fibro-obliterative lesion of PSC.
E) H&E, low power magnification – large bile duct with inspissated bile.
F) H&E, high power magnification – malignant glands consistent with cholangiocarcinoma arising in PSC.
Key points: Cirrhosis due to PSC.
1. Clinical history – young adult -> middle aged (M>F), ERCP with areas of bile duct structuring, history of inflammatory bowel disease (particularly ulcerative colitis).
2. Histology:
a. Onion skinning fibrosis and fibro-obliterative lesions - hepatocyte biliary metaplasia (CK7 immunostain).
b. Fibrosis – portal-based process with progression to macronodular “jigsaw” fibrosis.
c. Cholatestasis - Chronic cholestasis leads to cholatestasis - feathery degeneration of periportal hepatocytes which appear enlarged, swollen with clear/granular cytoplasm.
d. Risk of malignancy –> cholangiocarcinoma (hilar tissue entirely submitted).
Case #4: Portal fibrosis: chronic hepatitis C cirrhosis.
The patient is a 67-year-old with a history of cirrhosis due to chronic hepatitis C (treated), hepatocellular carcinoma (treated with TARE) and interstitial lung disease. The patient underwent liver transplant.
| Liver enzymes | |
| AST | 29 U/L |
| ALT | 10 U/L |
| ALKP | 100 U/L |
| TBILI | 1.3 mg/dL |
| ALBUMIN | 3.4 g/dL |
Liver explant:
Cirrhosis due to chronic hepatitis C – macronodular cirrhosis with regression.
A) H&E, low power magnification – macronodular cirrhosis with significant regression.
B) Trichrome, low power magnification – macronodular cirrhosis with significant regression.
Key points: Cirrhosis due to chronic hepatitis C.
1. Clinical history – clinical/serologic evidence of hepatitis C viral infection.
2. Histology:
a. Portal inflammation with interface activity (chronic hepatitis appearance).
b. Fibrosis – portal-based process with progression to cirrhosis.
c. Treated hepatitis C can result in regression of fibrous septae over time. Portal inflammation can linger.
Case #5: Irregular fibrosis: cardiac cirrhosis:
The patient is a 49-year-old with a history of hypertrophic cardiomyopathy complicated by chronic hepatic venous outflow obstruction with progression to liver dysfunction. The patient underwent combined liver & heart transplantation.
| Liver enzymes | |
| AST | 12 U/L |
| ALT | 7 U/L |
| ALKP | 188 U/L |
| TBILI | 0.6 mg/dL |
| ALBUMIN | 4.0 g/dL |
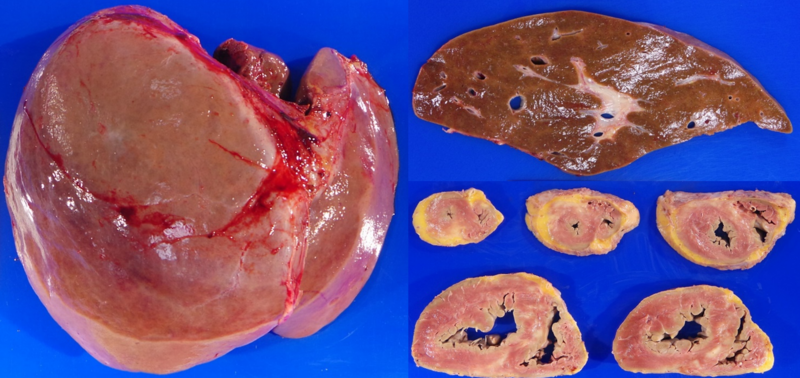
Liver explant:
Cardiac cirrhosis – irregular pattern of fibrosis, heart with hypertrophic cardiomyopathy.
A) and C) H&E, low power magnification – irregular pattern of cirrhosis.
B) and D) Trichrome, low power magnification – irregular pattern of cirrhosis.
Key points: Cirrhosis due to chronic hepatic venous outflow.
1. Clinical history – cardiac history (heart failure, cardiomyopathy, etc). Simultaneous heart and liver transplants.
2. Histology:
a. Sinusoidal dilation, congestion, assessment of fibrosis (on pre-transplant biopsy)
b. Fibrosis – centrilobular sinusoidal based process with progression to an irregular pattern of fibrosis.
Case #6: Irregular fibrosis: sickle cell hepatopathy:
The patient is a 32-year-old with a history of sickle cell anemia that presented with in sickle cell crisis with acute liver failure. The patient underwent a liver transplant.
| Liver enzymes | |
| AST | 540 U/L |
| ALT | 184 U/L |
| ALKP | 133 U/L |
| TBILI | 59.8 mg/dL |
| ALBUMIN | 2.6 g/dL |
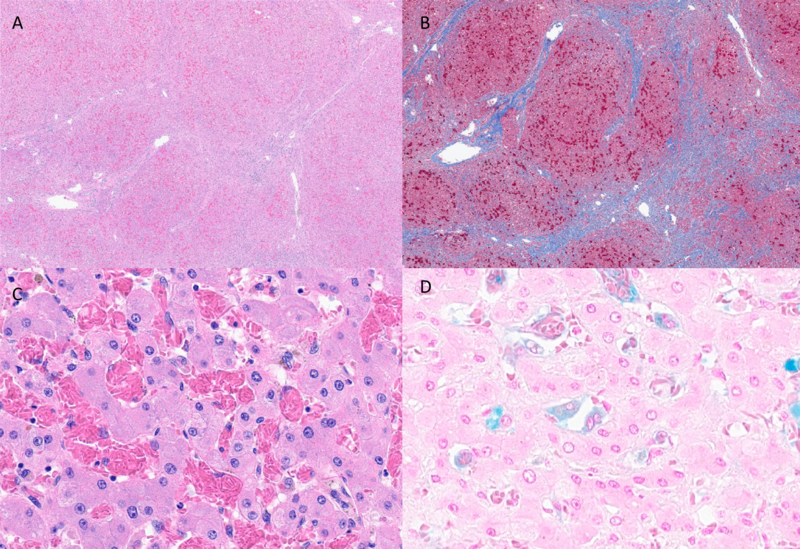
Liver explant:
Sickle cell hepatopathy cirrhosis – hepatomegaly with irregular pattern of fibrosis, green-black gallstones.
A) H&E, low power magnification – irregular pattern of cirrhosis.
B) Trichrome, low power magnification – irregular pattern of cirrhosis.
C) H&E, high power magnification – sinusoidal congestion with sickled red blood cells.
D) Prussian blue – iron stain showing secondary hemosiderosis with iron deposition in Kupffer cells.
Key points: Cirrhosis due to sickle cell hepatopathy.
1. Clinical history – sickle cell disease, inadequately managed with red cell transfusion/exchange.
2. Histology:
a. Congestion with sickled red blood cells, assessment of fibrosis.
b. Fibrosis – irregular pattern of fibrosis.
c. Secondary hemosiderosis due iron overload from red cell transfusions.