Hepatocellular Carcinoma Locoregional Therapies
Ablation Therapies
Radiofrequency ablation (RFA) uses alternating electric current applied to the target lesion through an electrode. The high temperature causes coagulative necrosis and cell death. RFA is limited by decreased efficacy at the periphery due to resultant eschar, which increases tissue impedance. There may also be incomplete ablation of perivascular tumors due to the heat-sink effect, with convection cooling from large vessels. RFA can additionally cause biliary complications, including biliary stricture and biloma.
Microwave ablation (MWA) uses electromagnetic energy to raise tissue temperature and deliver cellular injury. MWA allows for larger target area with more uniform ablation and delineated borders, compared to RFA. It is also less susceptible to convection cooling compared to RFA.
One systematic review reported similar mortality and major complications rates after RFA and MWA, 0.16% and 3.29%, respectively. Major complications included liver abscess, visceral injury, bleeding, and liver failure. Tumor seeding has been reported in both RFA and MWA, with increased risk when performed with biopsy. While one small study reported a tumor seeding rate of 12.5% with RFA, most studies have shown low (0.5-3%) risk after introduction of the coaxial needle technique. The risk of tumor seeding can be mitigated by coagulation of the needle tract upon withdrawal.
Other ablation techniques:
Percutaneous ethanol injection (PEI) is an early ablative technique used for treatment of early-stage HCC, and involves injection of ethanol into the tumor, resulting in coagulative necrosis. It is limited by less defined treatment margins and the need for prolonged or repeated sessions, and was showed to be inferior to RFA in local recurrence and overall survival.Cryoablation induces tumor necrosis by delivering subfreezing temperature to the tumor which causes direct physical damage, resulting in ischemia and infarction. However, cryoablation has a high complication rate, including cryoshock which involves multiorgan failure. Its use has decreased since the development of RFA and MWA. Irreversible electroporation (IRE) delivers high-voltage low energy current pulses to the tumor, inducing apoptosis of tumor cells. Its use is limited by the need for general anesthesia and cardiac gating to prevent cardiac arrhythmias.
Efficacy and indication:
Currently, AASLD, EASL and APASL guidelines recommend RFA or MWA as a first-line therapy for solitary tumors < 2 cm (BCLC 0).
Studies show that up to 94% of patients have complete tumor response after 1-3 sessions of RFA. Larger tumor size (>2.5-3 cm) was found to be a predictor of local recurrence but not of overall survival after RFA. While there is a theoretical advantage of MWA over RFA, randomized control trials have not shown differences in local recurrence, progression or overall survival. A recent phase III study showed improved recurrence-free survival using adjuvant atezolizumab and bevacizumab for one-year after ablation in patients at high risk of recurrence (size 2-5 cm or multifocality).
Transarterial therapies
During HCC carcinogenesis, there is development of arteries without paired veins, in contrast to normal hepatocytes which receive blood supply from both hepatic artery and portal vein. Transarterial embolization interrupts arterial blood supply to the tumor, which results in ischemic necrosis. The portal vein blood supply compensates this loss of arterial inflow to normal hepatocytes.
Transarterial chemoembolization (TACE) involves injection of embolizing microparticles and chemotherapeutic agents (usually doxorubicin), occluding the arterial supply of target lesion. TACE is generally repeated in 1-2-month intervals until complete response is achieved. Portal vein thrombosis was previously considered an absolute contraindication to TACE; however, recent data suggest that TACE can be safely performed in select patients with alterations in technique.
Drug-eluding beads have also been used with TACE (DEB-TACE), using polyvinylchloride microspheres pre-loaded with chemotherapeutic drug. This leads to a more sustained, prolonged and predictable release of drug, reducing the collateral systemic effects of chemotherapeutic agents and resulting in a more predictable arterial occlusion. Studies have not shown any difference in progression-free or overall survival between DEB-TACE and conventional TACE.
The most common complication of TACE is post-embolization syndrome, which has been reported in up to 40% of patients. It usually presents with nausea, fever, and abdominal pain, and severity may be associated with extent of ischemia in normal parenchyma, as well as underlying liver function. Other complications include liver decompensation, kidney injury, biliary injury, abscess, bleeding, and ischemic cholecystitis. Presence of a biliary-enteric anastomosis or a biliary stent increases the risk of hepatic abscess.
In transarterial radioembolization (TARE), radioactive particles (usually Yttrium-90 microspheres) are injected into the selected arterial branch. Beta radiation results in DNA double strand breaks and tumor cell damage. Post-embolization syndrome is the most common side effect, similar to the post-TACE syndrome. Other complications include radiation gastritis and gastrointestinal ulceration, cholecystitis, pancreatitis and pneumonitis. Radioembolization-induced liver disease (REILD) is a form of hepatic veno-occlusive disease that can be fatal. It is more common in patients with underlying cirrhosis or prior/subsequent exposure to chemotherapy. Modifications to standard protocol to more selectively apply TARE has been shown to reduce the incidence of REILD.
Efficacy and Indication:
AASLD, EASL, and APASL guidelines recommend TACE as first line for patients with intermediate stage HCC (BCLC stage B) – patients with multinodular disease, Child-Pugh class A or B cirrhosis, without portal vein invasion or extrahepatic disease. APASL and AASLD guidelines recommend TARE as an alternative to TACE.
TACE has been shown to increase survival in patients with unresectable HCC when compared best supportive care, with up to 63% survival at 2 years. TACE is commonly used for downstaging or bridging treatment for patients undergoing evaluation for transplant though there are no official guidelines recommend specific locoregional modalities for downstaging or bridging.
TARE has been shown to be a safe alternative to TACE. A meta-analysis of 553 patients with unresectable HCC with similar complication profile and overall survival. TARE has also been used for downstaging of HCC, with one study comparing TARE to TACE for downstaging of 86 UNOS T3 finding that TARE was superior to TACE, with 58% of TARE patients achieving downstaging to T2, and only 37% of TACE patients. In this study, TARE was also favored in response rate, time to progression, and overall survival, though these differences were not significantly significant. While TARE is not recommended as first line therapy in current guidelines, recent data is promising for TARE an alternative to TACE.
Radiation Therapy
Stereotactic body radiotherapy (SBRT) delivers high-dose external beam radiotherapy to the target tumor, with the goal of minimizing radiation to healthy surrounding parenchyma. Patients can experience radiation induced liver disease due to inevitable irradiation of non-target healthy liver parenchyma. Other complications include ulceration, perforation, stenosis, and biliary injury.
Practice guidelines acknowledge emerging literature showing promising outcomes for SBRT, but it has not yet been sufficiently validated to be recommended as a first-line treatment. Recent small prospective studies evaluating SBRT for early stage HCC show similar outcomes to reported outcomes for other locoregional therapies, with reported overall survival up to 78% at three years. One systematic review of 2846 patients who underwent SBRT showed 3 year local control and overall survival were 84.2% and 48.3% respectively. A few studies have used propensity score matching to compare SBRT to other modalities, with improved local control and similar overall survival when compared to TACE and RFA. Sapisochin et al compared patients who underwent SBRT, RFA, or TACE as bridging therapies prior to liver transplantation and found similar post-transplantation survival rates. Several trials comparing SBRT to other modalities are ongoing.
Combination Therapy
Combination of locoregional therapy, specifically TACE and RFA, has shown promising results in small studies. When TACE is performed prior to RFA, the limiting of hepatic artery flow by TACE theoretically decreases the heat sink effect, thus making RFA more effective. One retrospective study of patients with 2-3 cm solitary HCC found improved progression free survival with combination therapy compared to RFA alone. One single-center randomized control trial including patients with early stage HCC found improved overall survival and recurrence-free survival with combination therapy. High quality data evaluating TACE and RFA combination therapy is still lacking, and this strategy has not been adopted into standard practice.
Multiple studies are ongoing evaluating the efficacy of locoregional therapy in combination with systemic therapy, though have not shown improvement in outcomes thus far for HCC. DEB-TACE was studied in combination with Sorafenib in the TACE2 and SPACE randomized controlled trials, with no significant improvement in outcomes with combination therapy compared to DEB-TACE alone. TACE was combined with Sorafenib in the TACTICS trial, and did show improvement in progression-free survival, although this did not appear to translate into differences in overall survival. The SORAMIC trial compared TARE plus Sorafenib with Sorafenib alone, and no benefit was shown with addition of TARE. There is ongoing research evaluating the efficacy of combination locoregional and systemic therapy using immune checkpoint inhibitors.
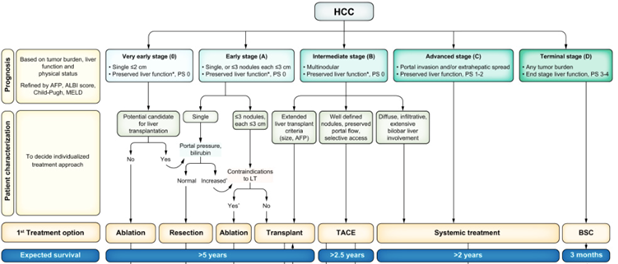
Adapted from “BCLC strategy for prognosis prediction and treatment recommendation: the 2022 update.”
Multidisciplinary Care in HCC
Management of HCC is increasingly complex, with prevalence of underlying liver disease and multiple treatment options by different specialties. Expert panels, including AASLD guidance documents, advocate for multidisciplinary care for patients with HCC. A multidisciplinary team for HCC usually includes hepatology, transplant surgery, medical oncology, radiology, interventional radiology, and radiation oncology. Some teams may also include palliative care, nutrition, and nursing. Multidisciplinary care helps to facilitate discussion between experts, individualize care, and optimize diagnosis, treatment and outcomes of patients.
Several studies have shown benefit in multidisciplinary care for patients with cancer. One systematic review and meta-analysis found that patients with HCC treated by a multidisciplinary team had significant improvement in overall survival and non-significant improvement in curative treatment receipt. With ongoing investigation into combination therapies, and recent promising data for use of immune checkpoint inhibitor therapy in earlier stages of HCC, multidisciplinary care is likely to become increasingly important.
Take Home Points
- Radiofrequency ablation is considered first-line therapy for very early-stage HCC (BCLC-0) and an alternative to surgical resection in early stage (BCLC-A) HCC. Recent data shows microwave ablation has similar results compared to radiofrequency ablation.
- Transarterial chemoembolization is considered first-line therapy for intermediate stage HCC and is effective in downstaging and bridging prior to liver transplantation. Recent data shows transarterial radioembolization has comparable outcomes, though it is not currently recommended as a first-line therapy.
- Stereotactic body radiotherapy has early data with encouraging results in patients with early and intermediate stage HCC, and in particular may be helpful in HCC that is not suitable for surgical resection or ablation.
- There is ongoing investigation into the combination of different locoregional therapies as well as with systemic therapies, though none yet adopted into standard practice.
- Multidisciplinary care can help to optimize diagnosis, treatment, and outcomes of patients with HCC.