Defining and Managing Acute Liver Failure
Learning points:
- Define acute liver failure and its contrast from chronic liver disease.
- Outline preliminary diagnostic workup to guide management of acute liver failure.
- Recognize the role of liver transplantation in managing acute liver failure.
Definition and diagnosis:
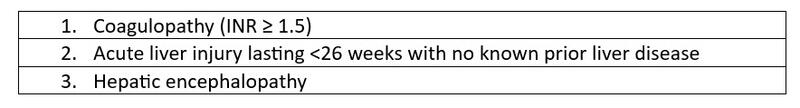
- Acute liver failure (ALF) is defined by the following criteria:
- Survival without liver transplantation varies on the etiology.
- Transplant-free survival for all-comers according to a large registry-based study was only 50%.
- Survival has increased significantly from 20% to greater than 60% in the past few decades due to improvements in supportive critical care and use of liver transplantation in selected patients à timely recognition of ALF is crucial!
Pathophysiology:
- The major risk of mortality in patients with ALF is cerebral edema
.- Seen in approximately 80% of patients with grade IV hepatic encephalopathy and can lead to herniation and death.
- Acutely elevated ammonia leads to astrocyte swelling and dysfunction leading to cerebral edema in ALF.
- The degree of arterial ammonia elevation in a patient correlates with the risk of cerebral edema.
- In patients with chronic liver disease or cirrhosis, the brain has time to create osmotic buffers over time to prevent severe cerebral edema to the point of herniation from hepatic encephalopathy.
- However, in ALF the flood of toxins including ammonia to the brain and the body does not have time to create this osmolar buffer to compensate due to the acuity.
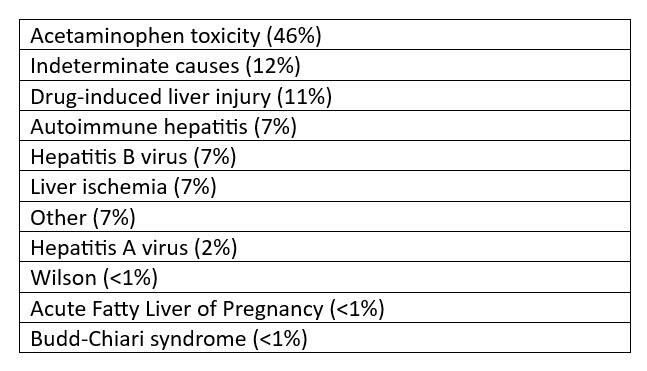
Common causes:
Common causes of ALF in the United States
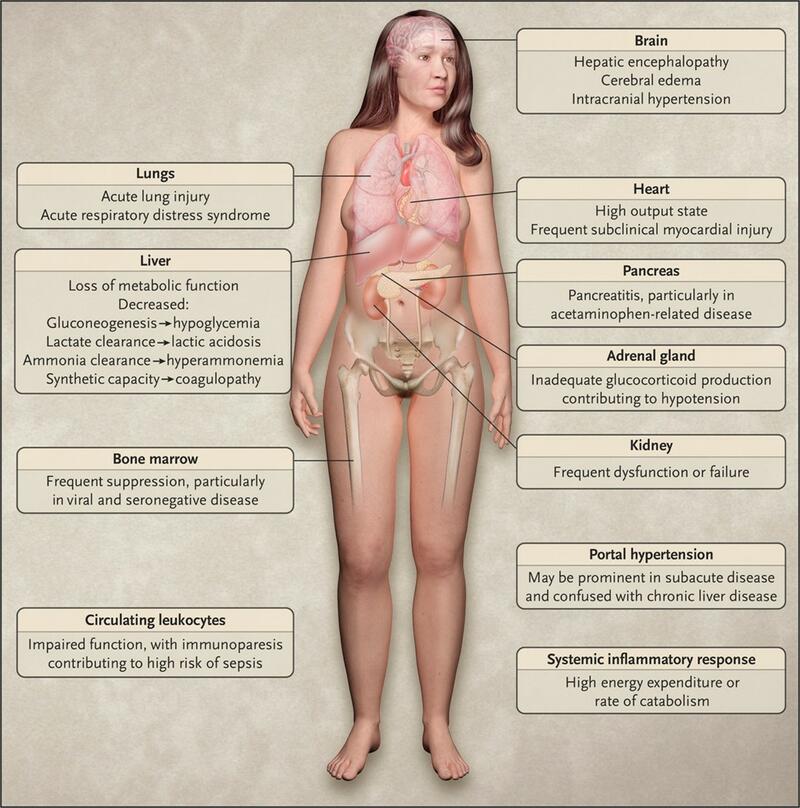
Clinical Manifestations:
- ALF can affect multiple organ systems. Symptoms usually start with a prodromal period of fatigue, nausea, vomiting, right upper quadrant pain, and jaundice, followed by multiorgan system organ failure as the time spent in liver failure progresses.
Figure: Multiorgan dysfunction in ALF
Diagnostic workup of ALF
- Historical clues are important to obtain from the patient or close contacts who can provide a history if the patient has encephalopathy and cannot provide a coherent history. Some important historical elements can include:
- Thorough medication reconciliation and inquiry of herbals or dietary supplements.
- High risk exposures for viral hepatitis.
- Past medical history of autoimmune disease (may favor autoimmune hepatitis), neuropsychiatric disease (can be a sign of Wilson’s Disease), substance use.
- Prior history of liver disease or jaundice, or prior records from other medical providers that include liver enzymes or liver imaging.
- The liver enzyme pattern can give preliminary clues to the etiology of ALF. For instance:
- Very high transaminase levels (≥3000 IU/L) may point towards viral hepatitis, acetaminophen overdose, or hepatic ischemia (especially if AST > ALT).
- DILI can present with any variety of enzyme patterns, but a primarily cholestatic picture is more worrisome.
- High liver enzymes with concurrent low alkaline phosphatase may point towards Wilson’s Disease.
- A comprehensive laboratory work up should be sent that evaluates the differential diagnosis and prepares for the prospect of a liver transplant evaluation.
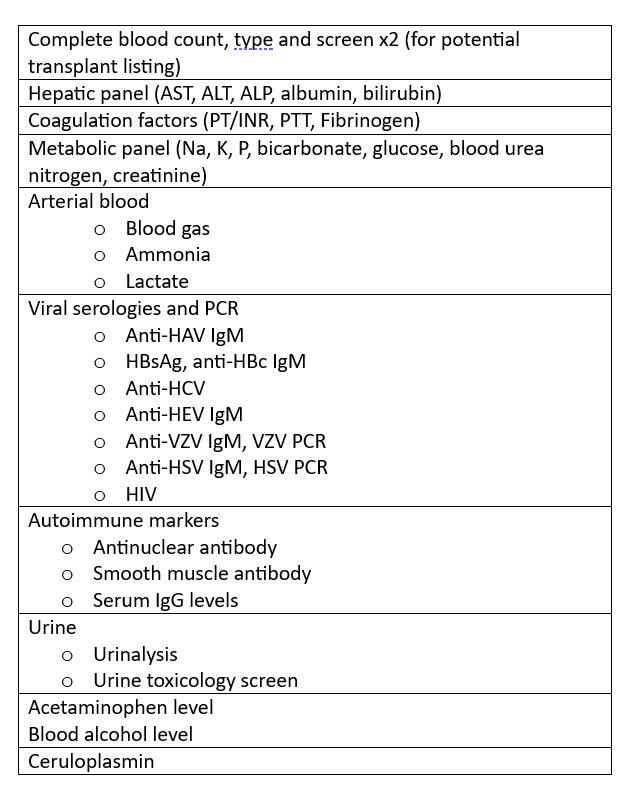
Repeated lab monitoring every few hours also helps with real-time prognostication of which patients may be improving with support, versus which are progressing and need timely transplant evaluation. These include:
- MELD labs
- Coagulation factors (INR, Fibrinogen)
- Arterial Ammonia, Lactate, pH
- Elevated AFP or low phosphorus levels can suggest liver regeneration
Role of liver biopsy
- Liver biopsy may be needed if the laboratory workup or imaging findings do not provide a specific etiology for ALF, however risks with bleeding should be taken into account. If a liver biopsy is needed, a transjugular approach is preferred to reduce bleeding risk. This should only be performed in evaluating indeterminate etiologies where performing a liver biopsy would change management.
Imaging:
- Cross-sectional abdominal imaging with contrast is ideal to survey the hepatic anatomy, vasculature, and inform potential surgical planning for liver transplantation; if this is not possible due to patient acuity, an ultrasound doppler of the liver at the patient’s bedside should be obtained in the interim.
Management:
- Empiric N-acetylcysteine (NAC) infusion is often started while awaiting workup for ALF. It is also the treatment of choice for acetaminophen toxicity.
- NAC also improves outcomes in non-acetaminophen ALF as some reports suggest it improves transplant-free survival if used in early-stages of ALF.
- Empiric IV acyclovir should be considered in cases with ALF of unknown etiology until herpes simplex virus (HSV) PCR testing returns. This mitigates the high mortality associated with HSV hepatitis.
- Neurological monitoring with serial neurological exams, and non-invasive measures of intracranial pressure measurement can be performed at the bedside
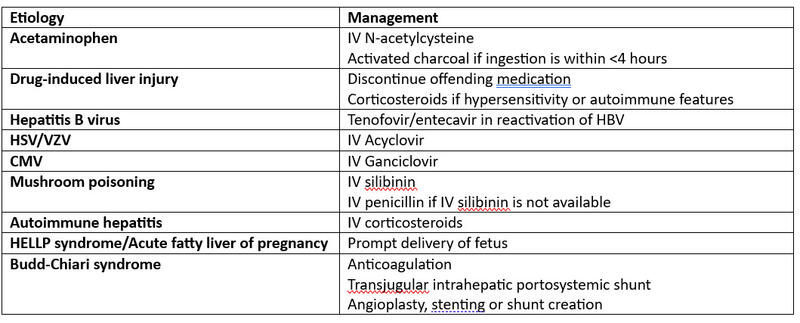
Etiology-specific management of ALF
Renal Replacement Therapy
- Acute kidney injury (AKI) is present in approximately 70% of patients with ALF, and approximately 30% of these patients require renal replacement therapy (RRT).
- Early RRT in the form of continuous hemofiltration, even in absence of AKI, can be considered in attempts to temporize the progression of hepatic encephalopathy through filtration of ammonia and other toxic substances.
- Continuous modes of RRT are preferred over intermittent modes to avoid a wider range of metabolic and hemodynamic fluctuations, which can increase cerebral edema and intracranial pressure.
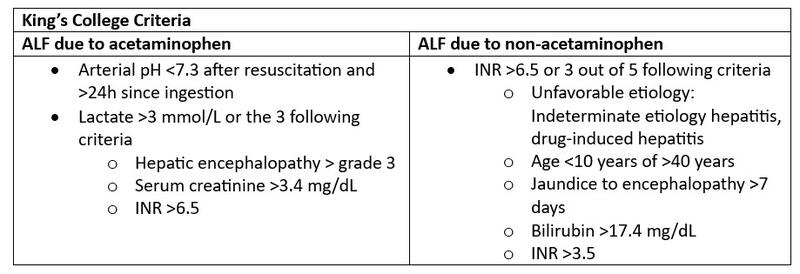
Prognostic scores and the role of LT for ALF
- Multiple prognostic scores have been developed for ALF. One of the most well-known and utilized is the King’s College Criteria (KCC).
- Although improvements in medical care have significantly lowered mortality rates, LT is being implemented in approximately 30% of patients with ALF, and offers a life-saving treatment.
- It is important that patients are transferred or cared for at a liver transplant center, and based on continuous, real-time clinical data, the decision to proceed with liver transplantation can be done while providing medical and supportive care.
- Patients who recover with medical treatment, as well as those with irreversible causes such as ischemic liver injury or too critically sick for transplant (shock, uncontrolled infection, cerebral herniation) are not considered candidates for LT.
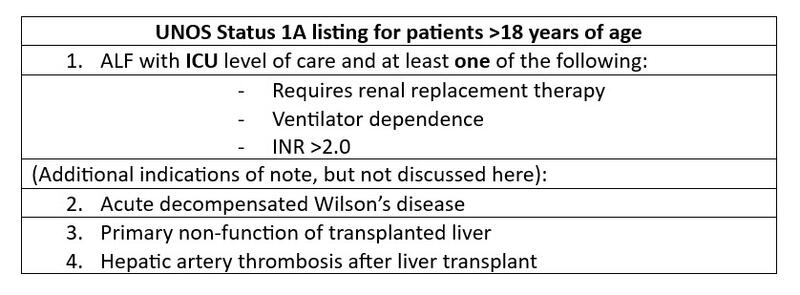
- For patients with ALF who are deemed transplant candidates, they are listed as “Status 1A” in UNOS which means they are at the top of the waitlist regardless of their MELD score.
Take Home Points
- ALF is severe liver injury with coagulopathy and hepatic encephalopathy in a patient with no known liver disease.
- Mortality in ALF is related to cerebral edema and progressive multi-organ dysfunction.
- Early referral to a LT center should be pursued as soon as ALF is clinically suspected in order to expedite transplant evaluation for patients who need it.