An Acute Severe Dilemma

Autoimmune hepatitis definitions
Taken from: Acute Severe Autoimmune Hepatitis: Corticosteroids or Liver Transplantation? Liver Transplantation 2019.
Establishing the Diagnosis of Acute Severe Autoimmune Hepatitis
Making a diagnosis of acute severe autoimmune hepatitis (AS-AIH) is critical to providing safe, rapid treatment. Because the treatment of choice is corticosteroids, which carry a risk of harmful side effects including infection, other conditions must be ruled out. Viral hepatitis can present similarly to AS-AIH, thus testing for hepatitis A, B, C, along with herpes simplex virus, Epstein-Barr virus, cytomegalovirus, varicella-zoster virus, and parvovirus should be carried out. In addition, hepatitis E virus testing, which is a rare mimicker of AS-AIH, must be excluded. Drug-induced liver injury, autoimmune cholangiopathy, Wilson's disease, and Budd-Chiari syndrome are other liver diseases that can present similarly. Along with excluding these other conditions, the diagnosis of AIH--if not already definitively diagnosed--can be secured with positive serologic markers such as anti-nuclear antibodies, anti-smooth muscle antibodies, or anti-liver kidney microsome antibodies, and a liver biopsy, which is the gold standard of diagnosis. Interface hepatitis, hepatocyte rosettes, and emperipolesis (one cell telescoping into another) are common histologic findings in AIH (Figure 2). Ultimately, there are gold standard criteria that incorporate labs, serology, and histology to diagnose AIH definitively.
Figure 1 - Spectrum of presentation for AIH.
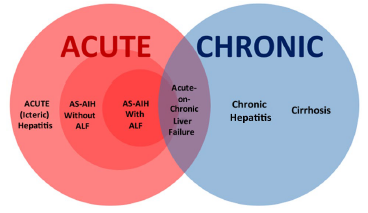
Taken from: Acute Severe Autoimmune Hepatitis: Corticosteroids or Liver Transplantation? Liver Transplantation 2019.
Figure 2 - Autoimmune hepatitis histology. A: interface hepatitis; B: interface hepatitis, magnified; C: necro-inflammatory lobular hepatitis; D: emperipolesis (arrow shows intracytoplasmic lymphocytes).

Taken from: Approach to the Patient with Acute Severe Autoimmune Hepatitis. JHEP Rep 2020.
Inpatient Management of Acute Severe AIH
The first line therapy for AS-AIH is corticosteroids. Response rates vary, ranging from 20%-100%. The recommended medication and dose is prednisolone 0.5-1mg/kg/day. Hospitalization is recommended for close monitoring not only for biochemical response but also for lack of clinical improvement and potential progression to acute liver failure. MELD labs once or twice daily should be measured, and if there is biochemical and clinical improvement by seven days, the steroids should be tapered and azathioprine can be considered as an adjunctive agent. The most crucial element of AS-AIH management is determining whether urgent liver transplant evaluation should be initiated. The development of hepatic encephalopathy or lack of biochemical response or improvement after one to two weeks of steroid therapy requires a consideration for liver transplant. Of note, statistically significant increases in sepsis have not been shown for AIH patients treated with steroids.

Figure 3 - Management algorithm for acute severe AIH.
Taken from: Acute Severe Autoimmune Hepatitis: Corticosteroids or Liver Transplantation? Liver Transplantation 2019.
